What Is Legionnaires’ Disease? A Comprehensive Guide to Causes, Symptoms, and Diagnosis
Contents
- 1 What Is Legionnaires’ Disease? A Comprehensive Guide to Causes, Symptoms, and Diagnosis
- 1.0.0.0.0.1 Read DISCLAIMER
- 1.0.0.0.0.2 The material presented here is for general informational and educational purposes only and is not medical advice. Although we attempt to provide current and accurate information, this blog should not be used as a replacement for professional medical consultation, diagnosis, or treatment. In all cases, consult your physician or an accredited medical practitioner with regards to any medical condition or treatment. Do not ignore professional medical advice or wait for it on the basis of information provided by this blog. In a medical emergency, call emergency services immediately.
- 1.1 Understanding the Invisible Threat
- 1.2 Origins and Biology of Legionella
- 1.3 Who Is at Risk—and Why
- 1.4 Recognizing the Symptoms: Subtle but Serious
- 1.5 How Legionnaires’ Disease Is Diagnosed
- 1.6 Treatment Options and Patient Support
- 1.7 Preventing Exposure: What Communities and Individuals Can Do
- 1.8 Identifying Myths vs. Facts About Legionnaires’ Disease
- 1.9 Recovery and Long-Term Outlook
- 1.10 Why Awareness and Infrastructure Matter Globally
- 1.11 Conclusion: Empowerment Through Understanding
- 1.12 FAQs with Answers
Discover what Legionnaires’ disease is, its symptoms, causes, and how it’s diagnosed. Learn how Legionella bacteria spreads through water systems and what steps you can take to prevent this severe form of pneumonia.
Read DISCLAIMER
The material presented here is for general informational and educational purposes only and is not medical advice. Although we attempt to provide current and accurate information, this blog should not be used as a replacement for professional medical consultation, diagnosis, or treatment. In all cases, consult your physician or an accredited medical practitioner with regards to any medical condition or treatment. Do not ignore professional medical advice or wait for it on the basis of information provided by this blog. In a medical emergency, call emergency services immediately.
Understanding the Invisible Threat
Legionnaires’ disease often lurks quietly in the background, mentioned only when outbreaks make headlines. Yet it’s not a myth—it’s a serious type of pneumonia caused by Legionella bacteria, usually found in water systems. The idea that a microscopic organism living in air conditioning units, hot tubs, or building plumbing can trigger deadly lung infections may seem surreal. And yet, across the world, people have become ill after inhaling mist or steam carrying these bacteria. What makes the disease especially concerning is its subtle onset, potential severity, and the way it preys on compromised immunity or aging physiology. But understanding how it spreads, manifests, and how it is diagnosed offers clarity—and with clarity comes better protection.
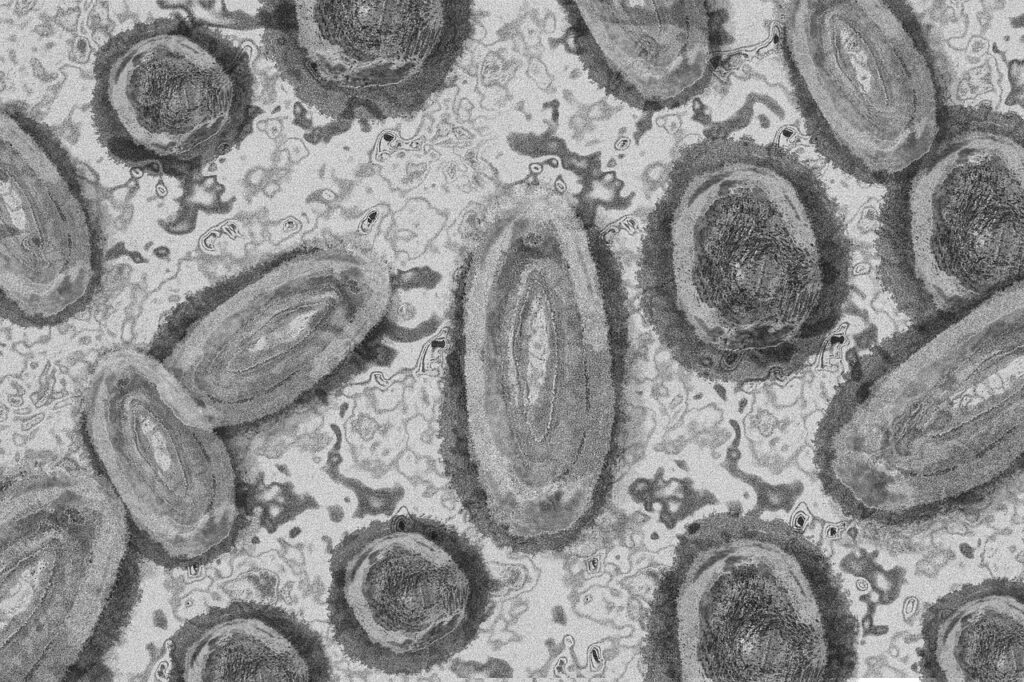
Origins and Biology of Legionella
Legionella pneumophila, the most common strain, thrives in warm, stagnant water between 20°C to 50°C (68°F to 122°F). Larger outbreaks have occurred in hotels, hospitals, office buildings, or cruise ships—anywhere water circulates through cooling towers, showers, decorative fountains, or hot tubs. Unlike viruses, Legionella isn’t transmitted from person to person. Instead, it infiltrates people via inhalation of contaminated water droplets, making infrastructure and maintenance a key battleground. In the lungs, these bacteria lodge in alveoli, replicate within immune cells, and trigger intense inflammation. This cascade of events results in lung tissue damage, systemic symptoms, and, in severe cases, organ dysfunction.
Who Is at Risk—and Why
Although anyone can be infected, the risk is higher in certain groups. Older adults, especially over 50, are more prone because of reduced lung resilience or chronic conditions. Smokers and people with chronic lung disease face greater vulnerability. Those with weakened immunity—due to transplant medications, cancer therapies, or chronic illnesses—face heightened risk as well. Yet even younger, healthy individuals have become severely ill when exposed to high bacterial loads or poorly maintained systems. The combination of environmental exposure and individual susceptibility sets the stage for serious infection.
Recognizing the Symptoms: Subtle but Serious
Symptoms commonly begin after a 2–10 day incubation period. Initially, people may experience fever, chills, dry cough, muscle aches, and headache. These early signs could easily be mistaken for flu or common pneumonia. Over time, symptoms escalate to include chest pain, shortness of breath, confusion, nausea, vomiting, diarrhea, and elevated heart rate. Some people develop hyponatremia (low sodium), acute kidney injury, or elevated liver enzymes. The mild flu-like phase often gives way to more severe, systemic illness—sometimes too rapidly to respond without hospitalization.

How Legionnaires’ Disease Is Diagnosed
Doctors often begin with suspicion based on symptoms and exposure history, especially in buildings with water systems or cooling towers. Blood tests may show elevated white cell counts, inflammatory markers, and renal or liver abnormalities. Chest X-rays or CT scans frequently reveal pneumonia-like infiltrates. Confirmation uses more specific tools: urine antigen tests detect Legionella-specific proteins; sputum cultures can isolate the bacteria; PCR assays detect bacterial DNA; and direct fluorescent antibody staining can visualize bacteria in respiratory samples. Because of varying sensitivity, multiple tests may be used to confirm diagnosis.
Treatment Options and Patient Support
Legionnaires’ disease is treated with antibiotics, primarily macrolides (like azithromycin) or fluoroquinolones (like levofloxacin). Intravenous administration is preferred for severe cases, with oral transition as patients improve. Early treatment is vital: starting therapy within 48 hours of symptom onset significantly reduces mortality. Supportive care—oxygen therapy, hydration, lung physiotherapy, and monitoring for complications like sepsis or kidney dysfunction—is equally important. Most hospitalized patients recover over a two-week period, but some need longer, and complications like fibrosis or lingering fatigue may persist.
Preventing Exposure: What Communities and Individuals Can Do
Prevention lies in proper water management. Buildings should maintain water systems at proper temperatures, disinfect cooling towers and plumbing, flush unused lines, and follow regularly updated Legionella control plans. Individuals can reduce exposure by avoiding steam rooms or fountains in poorly maintained facilities, allowing faucets to flush before use, and ensuring safe water handling in communal areas. Community awareness is also essential—public health agencies monitor water systems and report outbreaks to prevent clustering cases.
Identifying Myths vs. Facts About Legionnaires’ Disease
Many myths persist—some say it’s contagious between people, which is false. Others claim drinking contaminated water causes the disease—incorrect, since infection arises via inhalation, not ingestion. Some believe only large facilities get Legionella—but smaller offices or hotels with aging plumbing can, too. Knowledge dispels fear. The truth is that bacteria thrive in certain temperature ranges, and the critical factor is inhalation of microdroplets, not contact.
Recovery and Long-Term Outlook
Most individuals recover with appropriate treatment, though some—especially older patients or those with complications—face longer recovery, fatigue, or lung damage. Post-infection syndromes like reduced oxygen tolerance, muscle weakness, or cognitive slowing may last weeks or months. Follow-up chest imaging and pulmonary function tests help assess recovery. Rehabilitation, targeted respiratory therapy, and close monitoring can support a return to normal activity.
Why Awareness and Infrastructure Matter Globally
Legionnaires’ disease is not confined to certain countries or climates. With global interconnectedness and shared architectural designs, it’s a worldwide concern. As buildings age and water systems evolve, maintaining safe water practices matters more than ever. Healthcare professionals, building operators, and travelers all benefit from understanding Legionella’s transmission dynamics. Informed individuals help spark safer practices—by asking questions, demanding inspections, or recognizing symptoms early in themselves or loved ones.
Conclusion: Empowerment Through Understanding
Legionnaires’ disease combines hidden environmental risk with serious clinical implications. While it can feel invisible, its impact becomes very real in hospitals, rehabilitation centers, and buildings with outdated water systems. Yet knowledge brings control: we can implement preventive water management, seek care early if symptoms arise, and push for safer infrastructure policies. A natural organism doesn’t define fear—it defines responsibility and shared awareness. With science, empathy, and caution, we can coexist with our built environments safely and confidently.
FAQs with Answers
- What is Legionnaires’ disease?
Legionnaires’ disease is a severe lung infection (a type of pneumonia) caused by the Legionella bacteria, usually contracted by inhaling contaminated water droplets. - What causes Legionnaires’ disease?
It is caused by Legionella bacteria, commonly found in water systems like cooling towers, hot tubs, and plumbing systems where water sits and becomes aerosolized. - Is Legionnaires’ disease contagious?
No, Legionnaires’ disease does not spread from person to person; it is typically contracted through inhalation of airborne contaminated water droplets. - What are the early symptoms of Legionnaires’ disease?
Early symptoms include high fever, chills, cough, muscle aches, and headache, often resembling flu before progressing to pneumonia. - How is Legionnaires’ disease diagnosed?
It is diagnosed using a combination of chest X-rays, urine antigen tests for Legionella, and sputum culture tests to identify the bacteria. - Who is most at risk for Legionnaires’ disease?
Elderly individuals, smokers, people with chronic lung diseases, and those with weakened immune systems are at highest risk. - Can you get Legionnaires’ disease from drinking water?
No, drinking contaminated water typically does not cause the disease; it’s the inhalation of aerosolized water that poses a risk. - What is the treatment for Legionnaires’ disease?
Antibiotics, particularly macrolides or fluoroquinolones, are the primary treatment and are often effective if administered early. - What happens if Legionnaires’ disease goes untreated?
Without treatment, it can lead to serious complications such as respiratory failure, septic shock, and death, especially in vulnerable populations. - How long does it take for symptoms to appear?
Symptoms usually appear 2–10 days after exposure to the Legionella bacteria. - Are there long-term effects of Legionnaires’ disease?
Yes, some people may experience lingering fatigue, respiratory issues, or neurological symptoms for weeks or months after recovery. - Can Legionnaires’ disease be prevented?
Yes, through proper maintenance of water systems, including regular disinfection and temperature control to prevent bacterial growth. - How common is Legionnaires’ disease?
While not extremely common, it is on the rise in many countries due to aging infrastructure and increased use of complex water systems. - Is there a vaccine for Legionnaires’ disease?
No, currently there is no vaccine available for the prevention of Legionnaires’ disease. - What industries are at higher risk for outbreaks?
Healthcare facilities, hotels, cruise ships, and large commercial buildings with complex water systems are more prone to outbreaks if not properly maintained.

That analysis is spot on! Seeing how platforms like slotmax game use probability is fascinating. Makes you think about strategy, even in games of chance! Definitely checking out their login options.
Please tell me more about this. May I ask you a question? http://www.kayswell.com
Thank you for providing me with these article examples. May I ask you a question? http://www.kayswell.com
Thank you for sharing this article with me. It helped me a lot and I love it. http://www.kayswell.com
You’ve been great to me. Thank you! http://www.kayswell.com
I am not sure where you are getting your info, but good topic. I needs to spend some time learning more or understanding more. Thanks for excellent info I was looking for this information for my mission. http://www.kayswell.com
Hello, I enjoy reading through your article. I wanted to write a little comment to support you. http://www.kayswell.com
You should be a part of a contest for one of the finest blogs on the net. I’m going to highly recommend this blog! http://www.kayswell.com
Need a quick link to 368bet? link368bet seems to do the trick. Sometimes those other sites are blocked, so it’s handy to have a backup. Worth bookmarking, yeah? Check out link368bet if you’re having trouble getting through.
RBVN is eh, a site. I’ve logged in. You can also. I dunno! Try it if you want! rbvn
Fala, apostadores! Tô buscando um app novo pra dar uns palpites e me indicaram o DonaldBetApp. Alguém usa? Acha que vale a pena baixar? Me contem! Se quiserem saber mais: donaldbetapp
Carbon credits https://offset8capital.com and natural capital – climate projects, ESG analytics and transparent emission compensation mechanisms with long-term impact.
Свежие новости SEO https://seovestnik.ru и IT-индустрии — алгоритмы, ранжирование, веб-разработка, кибербезопасность и цифровые инструменты для бизнеса.
Бассейн сделать под ключ https://atlapool.ru
Хочешь помочь своей стране? подписать контракт на сво онлайн военную требования, документы, порядок заключения контракта и меры поддержки. Условия выплат и социальных гарантий.
Все подробности по ссылке: https://headacheclinic.ru/
Лучшие казино без депозита — бесплатные бонусы для старта, подробные обзоры и сравнение условий различных платформ.
Нужны казино бонусы? новые промокоды казино — бонусы за регистрацию и пополнение счета. Обзоры предложений и подробные правила использования кодов.
Онлайн покер покерок официальный сайт — турниры с крупными гарантиями, кеш-игры и специальные предложения для игроков. Обзоры форматов и условий участия.
I will right away snatch your rss as I can not find your email subscription link or e-newsletter service. Do you have any? Kindly let me understand in order that I may just subscribe. Thanks.
Все о фундаменте https://rus-fundament.ru виды оснований, расчет нагрузки, выбор материалов и этапы строительства. Практичные советы по заливке ленточного, плитного и свайного фундамента.
Все о ремонте квартир https://belstroyteh.ru и отделке помещений — практические инструкции, обзоры материалов и современные решения для интерьера.
Зарубежная недвижимость https://realtyz.ru актуальные предложения в Европе, Азии и на побережье. Информация о ценах, налогах, ВНЖ и инвестиционных возможностях.
Всё про строительство https://hotimsvoydom.ru и ремонт — проекты домов, фундаменты, кровля, инженерные системы и отделка. Практичные советы, инструкции и современные технологии.
Найкращі бонусы казино — депозитні акції, бездепозитні пропозиції та турніри із призами. Огляди та порівняння умов участі.
Грати в найкраще казіно ігри — широкий вибір автоматів та настільних ігор, вітальні бонуси та спеціальні пропозиції. Дізнайтеся про умови участі та актуальні акції.
Онлайн ігри в казино – великий вибір автоматів, рулетки та покеру з бонусами та акціями. Огляди, новинки та спеціальні пропозиції.
Онлайн покер Покер онлайн pokerok — регулярные турниры, кеш-игры и специальные предложения для игроков. Обзоры возможностей платформы и условий участия.
ойын автоматы Mine Drop бонус ойыны ?алай ж?мыс істейді – т?пн?с?а т?жырымдамасы мен жар?ын дизайны бар динамикалы? ойын автоматы. Механика, бонусты? м?мкіндіктер ж?не ойын процесіні? м?мкіндіктері туралы білі?із.
A catalog of cars http://www.auto.ae/catalog/ across all brands and generations—specs, engines, trim levels, and real market prices. Compare models and choose the best option.
Un sito web https://www.sopicks.it per trovare abbigliamento, accessori e prodotti alla moda con un motore di ricerca intelligente. Trova articoli per foto, marca, stile o tendenza, confronta le offerte dei negozi e crea look personalizzati in modo rapido e semplice.
Siatkowka w Polsce http://www.siatkowkanews.pl najnowsze wiadomosci, wyniki meczow, terminarze i transfery druzyn. Sledz PlusLige, wystepy reprezentacji narodowych i najwazniejsze wydarzenia sezonu w jednej wygodnej sekcji sportowej.
Jan Blachowicz https://janblachowicz.pl/ to polski zawodnik MMA i byly mistrz UFC w wadze polciezkiej. Pelna biografia, historia kariery, statystyki zwyciestw i porazek, najlepsze walki i aktualne wyniki.
IDMAN TV idman tv live stream online: watch the channel in high quality, check today’s program guide, and find the latest TV schedule. Conveniently watch sporting events and your favorite shows live.
Everything about FC Qarabag https://qarabag.com.az in one place: match results and schedule, Premier League standings, squads and player stats, transfers, live streams, and home ticket sales.
Free online games http://www.oyun-oyna.com.az with no installation required—play instantly in your browser. A wide selection of genres: arcade, racing, strategy, puzzle, and multiplayer games are available in one click.
Watch Selcuksport TV http://www.selcuksports.com.az/ live online in high quality. Check the broadcast schedule, follow sporting events, and watch matches live on a convenient platform.
Julie Cash juliecash.online on OnlyFans features exclusive content, private posts, and regular updates for subscribers. Subscribe to gain access to original content and special offers.
Crystal Lust https://crystal-lust.online is the official website, featuring original publications, premium content, and special updates for subscribers. Stay up-to-date with new posts and gain access to exclusive content.
Exclusivo de Candy Love https://candylove.es contenido original, publicaciones vibrantes. Suscribete para ser el primero en enterarte de las nuevas publicaciones y acceder a actualizaciones privadas.
Brooke Tilli https://brooketilli.online official website features unique, intimate content, exclusive publications, and revealing updates. Access original content and the latest news on the official platform.
Shilpa Sethi https://shilpasethi.in exclusive content, breaking news, and regular updates. Get access to new publications and stay up-to-date on the most interesting events.
MiniTinah minitinah comparte contenido exclusivo y las ultimas noticias. Siguenos en Instagram y Twitter para enterarte antes que nadie de nuestras nuevas publicaciones y recibir actualizaciones emocionantes a diario.
Eva Elfie https://evaelfie.ing shares unique intimate content and new publications. Her official page features original materials, updates, and exclusive offers for subscribers.
Lily Phillips http://www.lily-phillips.com/ offers unique intimate content, exclusive publications, and revealing updates for subscribers. Stay up-to-date with new content, access to original photos, and special announcements on her official page.
Unique content from Angela White https://angelawhite.ing new publications, exclusive materials, and personalized updates. Stay up-to-date with new posts and access exclusive content.
Sweetie Fox http://www.sweetiefox.ing/ offers exclusive content, original publications, and regular updates. Get access to new materials, private photos, and special announcements on the official page.
Souzan Halabi souzan halabi shares exclusive content and new publications. Get access to private updates and original materials on the official platform.
Riley Reid http://www.rileyreid.ing/ is a space for exclusive content, featuring candid original material and regular updates. Get access to new publications and stay up-to-date on the hottest announcements.
Shilpa Sethi shilpasethi.in official page features unique, intimate content and premium publications. Private updates, fresh photos, and personal announcements are available to subscribers.
Brianna Beach’s exclusive https://briannabeach.online page features personal content, fresh posts, and the chance to stay up-to-date on new photos and videos.
Luiza Marcato Official http://www.luizamarcato.online/ exclusive updates, personal publications, and the opportunity to connect. Get access to unique content and official announcements.
Exclusive Aeries Steele https://www.aeriessteele.online intimate content, and original publications all in one place. New materials, special announcements, and regular updates for those who appreciate a premium format.
Sabrina Cortez sabrinacortez offers unique content and fresh publications. Join us on social media to receive exclusive updates and participate in exciting activities.
Google salaries by position https://salarydatahub.uk comparison of income, base salary, and benefits. Analysis of compensation packages and career paths at the tech company.
Exclusive content Alexis Fawx alexisfawx original publications and special updates. Follow us on social media to stay up-to-date on new releases and participate in exciting events.
Любишь азарт? https://eva-vlg.ru онлайн-платформа с широким выбором слотов, настольных игр и живого казино. Бонусы для новых игроков, акции, турниры и удобные способы пополнения счета доступны круглосуточно.
Bunny Madison https://bunnymadison.online features exclusive, intimate content, and special announcements. Join us on social media to receive unique content and participate in exciting events.
Jill Kassidy Exclusives jillkassidy official online featuring original content, media updates, and special announcements.
Discover Avi Love’s avilove online world: exclusive videos, photos, and premium content on OnlyFans and other platforms.
Scarlett Jones scarlettjones.in shares exclusive content and the latest updates. Follow her on Twitter to stay up-to-date with new publications and participate in exciting media events.
Die Welt von Monalita monalita.de bietet exklusive Videos, ausdrucksstarke Fotos und Premium-Inhalte auf OnlyFans und anderen beliebten Plattformen. Abonniere den Kanal, um als Erster neue Inhalte und besondere Updates zu erhalten.
Johnny Sins johnny-sins.com is the official channel for news, media updates, and exclusive content. Be the first to know about new releases and stay up-to-date on current events.
Текущие рекомендации: оборудование для конференц залов
Discover the world of LexiLore https://lexilore.ing exclusive videos, original photos, and vibrant content. Regular updates, new publications, and special content for subscribers.
Serenity Cox https://www.serenitycox.ing shares exclusive content and regular updates. Follow her on Instagram, Twitter, and Telegram to stay up-to-date on creative projects and inspiring events.
Dive into the world of Dolly Little https://dollylittle-official.online original videos, exclusive photos, and unique content available on OnlyFans and other services. Regular updates and fresh publications for subscribers.
Купить квартиру https://sbpdomik.ru актуальные предложения на рынке недвижимости. Новостройки и вторичное жильё, удобный поиск по цене, району и площади. Подберите идеальную квартиру для жизни или инвестиций.
Karely Ruiz karelyruiz.mx comparte contenido exclusivo y actualizaciones periodicas. Siguela en Instagram, Twitter y Telegram para estar al tanto de sus proyectos creativos y eventos inspiradores.
Discover the world of Comatozze comatozze.in exclusive content on OnlyFans and active updates on social media. Subscribe to stay up-to-date on new publications and exciting projects.
Get to know JakKnife jak knife and discover unique content. Regular updates, special publications, and timely announcements are available to subscribers.
The official website of MiniTina https://www.minitinah.com your virtual friend with exclusive publications, personal updates, and exciting content. Follow the news and stay connected in a cozy online space.
Нужна плитка? тротуарная плитка город большой ассортимент, современные формы и долговечные материалы. Подходит для мощения тротуаров, площадок и придомовых территорий.
At online casino spain you can enjoy a very immersive atmosphere with localized themes that resonate well with the Spanish audience. The bonuses are transparent and easy to track within your personal account.
Строишь дом или забор? https://gazobeton-krasnodar.ru продажа газобетона и газоблоков в Краснодаре с доставкой по Краснодарскому краю и СКФО. В наличии автоклавные газобетонные блоки D400, D500, D600, опт и розница, расчет объема, цены от производителя, доставка на объект манипулятором
Нужен газоблок? https://gazobeton-krasnodar.ru/katalog/ каталог газоблоков и газобетона в Краснодаре: размеры, характеристики и цены на газобетонные блоки КСМК. Можно купить газоблоки с доставкой по Краснодару, краю и СКФО. Актуальная цена газоблоков, помощь в подборе, расчет объема и заказ с завода
Нужны ЖБИ? кольца бетонные для канализации широкий ассортимент ЖБИ, прочные конструкции и оперативная доставка на объект. Консультации специалистов и индивидуальные условия сотрудничества.
Visiting legal gambling chile gives you access to a legitimate gaming platform with clear terms and conditions regarding bonuses. The registration is fast, and the verification process didn’t take more than a few hours in my case.
Unique content from Gattouz0 Officiall – daily reviews, new materials, and the opportunity for personal interaction. Stay connected and get access to the latest publications.
Discover the world of Candy Love: exclusive content, daily reviews, and direct communication. Subscribe to receive the latest updates and stay up-to-date with new publications.
Contenido exclusivo de KarelyRuizOfficially: resenas diarias, nuevos materiales y la oportunidad de interactuar personalmente. Mantengase conectado y acceda a las ultimas publicaciones.
Immerse yourself in the world of Crystal Lust: unique content, daily reviews, and direct interaction. Here you’ll find not only content but also live, informal communication.
Exclusive from Sky Bri – daily reviews, new publications, and direct communication. Subscribe to stay up-to-date and in the know.
official page Elle Lee features hot posts, private selfies, and real-life videos. Subscribe to receive daily updates and exclusive content.
The official Lexis Star page features daily breaking news, personal selfies, and intriguing content. Subscribe to stay up-to-date with new updates.
The official delux_girlOfficiall channel features daily hot content, private selfies, and exclusive videos. Intriguing real-life moments and regular updates for those who want to get closer.
Discover the world of Naomi Hughes: daily vibrant content, candid selfies, and dynamic videos. Real life moments and regular updates for those who appreciate a lively format.
Discover the world of MickLiter Official: behind-the-scenes stories, bold provocations, and personal footage. All the most interesting content gathered in one place with regular updates.
intriguing publications Reislin and new materials appear regularly, creating a truly immersive experience. Personal moments, striking provocations, and unexpected materials are featured. Stay tuned for new publications.
Descubre el mundo de LiaLin: historias tras bambalinas, provocaciones audaces y videos personales. Todo el contenido mas interesante reunido en un solo lugar con actualizaciones periodicas.
Immerse yourself in the Mew Slut experience: candid behind-the-scenes moments, provocative vibes, and intriguing updates all in one place.
The best of MilaSolana – sharing all the most interesting content in one channel. Behind-the-scenes atmosphere, provocative mood, and personal snippets. Stay tuned and don’t miss any new releases.
exclusive revelations Monalita genuine passion and bold aesthetics. Private content you’ll find only here—directly from the author, without filters or unnecessary boundaries.
passionate atmosphere Amadani openness and a personal format of communication. Exclusive content, created without intermediaries—only for those who want more.
honest revelations AlinaRaiOfficial vivid emotions and a sensual atmosphere. Unique private content, available only on this page—directly from me.
bold format BigTittyGothEgg Officiall sincere emotions and expressive images. Private materials and special publications that you’ll only see here.
personal revelations EvaElfie Officially powerful energy and private publications. Unique content, available exclusively here—directly from me.
Genuine emotions GirthmasterrOfficiall bold visual presentation, and personal communication. Exclusive content revealed only to its audience.
Pure emotion Reislin Officiall bold presentation, and a private format without boundaries. Exclusive content, personally created and available only here—for those who appreciate true energy.
Candid style DianaRiderOfficiall vibrant passion, and a unique atmosphere. Private publications and unique materials that you’ll find exclusively in this space.
Vivid revelations Sweetie fox sensual aesthetics, and a signature format. Private materials created without boundaries or templates—available only in one place.
Pure emotion Reislin bold presentation, and a private format without boundaries. Exclusive content, personally created and available only here—for those who appreciate true energy.
Candid style DianaRiderOfficiall vibrant passion, and a unique atmosphere. Private publications and unique materials that you’ll find exclusively in this space.
Boldness and sincerity Luna Okko maximum intimacy. Personal content without intermediaries—only here and only directly from me.
Maximum candor Princess lsi vibrant energy, and a private atmosphere. Exclusive content is personally created and available only here—for those ready for a truly unique experience.
A bold image LunaOkkoOfficiall strong charisma, and a personal communication format. Private publications and special materials revealed only to our audience.
Frank emotions Rae Lil Blac captivating aesthetics, and a personalized format. Content without unnecessary filters—directly from the author.
The energy of passion Romi Rain sincerity, and private access. Unique publications created for those who appreciate a personalized and bold format.
Bold aesthetics SiriDahl Officiall personal revelations, and an intimate atmosphere. Exclusive content is created without compromise—only for our audience, and only here.
Sensual style CocoLovelock Officiall vibrant energy, and an unfiltered format. Unique materials available exclusively in this space.
Лучшее казино онлайн https://detsad47kamyshin.ru слоты, джекпоты, карточные игры и лайв-трансляции. Специальные предложения для новых и постоянных пользователей, акции и турниры каждый день.
Нужен компрессор? фильтр для компрессора для производства и мастерских. Надёжные системы сжатого воздуха, гарантия, монтаж и техническая поддержка на всех этапах эксплуатации.
Play unblocked games online without registration or downloading. A large catalog of games across various genres is available right in your browser at any time.
Работаешь с авито? авито бизнес аккаунт профессиональное создание и оформление Авито-магазина, настройка бизнес-аккаунта и комплексное ведение. Поможем увеличить охват, повысить конверсию и масштабировать продажи.
Подробности по ссылке: Медицинский массаж рядом: здоровье и релаксация в шаговой доступности
thc chocolate delivery in prague buy thc vape in prague
buy thc chocolate in prague buy thc vape in prague
cannabis thc gummies delivery in prague
420 store in prague 420 movement in prague
kush buy hash in prague
hash shop in prague cali weed for sale in prague
marijuana delivery in prague kush
hash in prague thc chocolate shop in prague
420 day in prague thc joint delivery in prague
buy kush in prague buy marijuana in prague
thc joint delivery in prague thc vape delivery in prague
buy thc vape in prague 420 movement in prague
hemp shop in prague thc gummies delivery in prague
cannabis store in prague cali weed shop in prague
buy hash in prague thc chocolate delivery in prague
cannabis store in prague marijuana delivery in prague
hash for sale in prague hash for sale in prague
thc gummies for sale in prague hashish in prague
buy thc joint in prague weed store in prague
Jouez-vous au casino? https://sultan-willd-fr.eu.com une plateforme de jeux moderne proposant une variete de machines a sous, de jackpots et de jeux de table. Inscription et acces faciles depuis n’importe quel appareil.
Check this site for essential information regarding local community initiatives and the strategic goals set by leadership. The layout is very clear, which makes it easy to find specific data about upcoming public events and policy updates without much effort. It really helps bridge the gap by providing transparent and timely information that matters to every active citizen in the region.
Visit here to find unique entertainment tips and detailed guides about the latest lifestyle trends. This platform is well-researched and provides a fresh perspective for anyone interested in high-quality content that isn’t covered by mainstream blogs. I especially like how they categorize their posts, making it easy to navigate through different themes without feeling overwhelmed.
At official casino portal you will find an extensive library of licensed slots and live dealer tables that definitely cater to all types of players. The site has a reputation for offering very competitive bonuses with fair wagering requirements, making it a solid choice for both beginners and pros. I’ve personally found their withdrawal process to be quite efficient, which is always a top priority when choosing a new platform.
Try Mr.Jackbet casino if you are looking for the official Mr.Jackbet platform with the most reliable slots and betting options. This destination is very professional and provides all the necessary details and service descriptions you might need before you start playing for real. It’s a great example of a secure environment that values transparency and makes it easy for users to find exactly what they need.
Inside 1xBet India casino you will find a massive selection of games specifically tailored for the Indian market, including hits like Teen Patti and Andar Bahar. The platform utilizes high-level encryption to ensure all transactions and personal data remain secure at all times. I also found that they offer excellent local deposit options, which makes the whole experience much more convenient for users in the region.
At Amunra login players in the Czech region can experience high-quality slots and live dealer games in a completely secure and localized environment. The site supports popular local payment methods and offers 24/7 customer support to resolve any technical or account issues as quickly as possible. It’s a very reliable destination for those looking for a smooth registration process and a diverse library of certified casino games.
On Boomerang official site you can enjoy a very engaging loyalty program that rewards active players with frequent cashback and exclusive tournament invitations. The platform is highly stable and performs well on both desktop and mobile browsers, ensuring you never miss a beat. It’s a great choice for those who value long-term rewards and a consistent gaming environment with plenty of variety.
Playing Plinko game online is a fantastic way to experience this classic arcade-style game with modern graphics and certified fair mechanics. The interface is very straightforward, allowing you to jump straight into the action without dealing with overly complicated settings or menus. It’s perfect for those who enjoy quick gaming sessions where the outcome is clear and the gameplay remains consistently engaging.
Visit official Sportuna link if you are looking for a premium gaming experience in Greece with a heavy focus on sports-themed slots and live betting. The site is fully localized, making navigation easy for Greek speakers, and the bonus offers are quite generous for new registrations. They have a great mix of classic casino games and modern sportsbook features that keep the overall experience very diverse.
Visiting Spanish tech portal is essential for those tracking the latest digital trends and platform launches in Spain for the upcoming year. The site provides technical details and roadmap updates that are quite valuable for anyone involved in the local tech or gaming sectors. It serves as an official hub for news and announcements regarding several key digital initiatives starting in early 2024.
Check https://fabersingt.com/gomblingo-casino/ for an expert analysis of the site’s payout speeds and the overall quality of their customer support team. This comprehensive guide covers everything from the registration process to the specific terms of their latest promotional offers. It’s an essential read for players who want to ensure they are joining a reliable platform with a strong track record.
Visiting best player site gives you a detailed look into the career and professional achievements of one of Mexico’s top football stars. The site includes exclusive content, career milestones, and regular updates that are perfect for dedicated fans of the midfielder. It’s a well-organized tribute to his journey from local clubs to the international stage and his ongoing impact on the sport.
On top Mexico news you will find a wide range of articles covering everything from local football to international sports tournaments. It’s a comprehensive portal for anyone who wants to stay updated on Mexican sports without having to visit multiple different news sites. The quality of the reporting is very high, and they cover a diverse range of athletic disciplines beyond just soccer.
Explore Mexico betting tips to find professional analysis and data-driven predictions for all major sporting events in the region. The site uses advanced statistical models to help users make more informed decisions when placing their bets on football, baseball, or other popular sports. It’s a great starting point for anyone looking to add a layer of expert insight to their wagering strategy.
This Monterrey news portal portal provides comprehensive coverage of the club’s history, current roster, and community initiatives in the Monterrey region. I check it regularly for official injury reports and transfer news to stay updated on the team’s latest developments. It’s a great resource for dedicated supporters who want to follow every aspect of the club’s journey in the league.
The https://365bet.com.mx/casino/ section offers a wide variety of classic games and new releases that are fully compliant with Mexican regulations. I’ve found their live dealer lobby to be one of the most professional in the region, featuring native-speaking dealers and high-definition streams. It’s a very secure environment where you can enjoy your favorite slots with peace of mind.
See official Toluca site for the most accurate statistics and official statements directly from the club’s management this season. The site offers a detailed look at the team’s performance metrics and upcoming match analysis, which is perfect for fans who like to dive deep into the numbers. It’s a professional and well-maintained site that serves as the official voice of the team for its loyal fanbase.
Checking official team portal is a must for any fan looking for the latest news, match schedules, and official team updates. The portal provides in-depth coverage of the club’s performance and includes exclusive interviews with players and coaching staff throughout the season. It’s the most reliable source for verified information regarding upcoming fixtures and official club announcements.
Using official gambling guide ensures that you are only accessing verified and licensed operators that fully comply with local Mexican laws. This guide is essential for players who prioritize financial security and want to avoid offshore sites with questionable reputations. It provides a clear list of legal platforms and explains the current regulations in a way that is very easy to understand.
порно студентки купить набор для мефедрона
порно вк порно онлайн бесплатно смотря
грузчик с ежедневной оплатой заказ грузчиков недорого
газель с грузчиками где найти грузчиков
Медицинская мебель https://tenchat.ru/0614265/ это основа оснащения клиник, лабораторий и частных кабинетов. Мы предлагаем мебель медицинская для любых задач: шкафы, столы, тумбы, стеллажи и специализированные решения. В ассортименте можно купить медецинскую мебель, соответствующая санитарным требованиям и стандартам безопасности.
Play online http://www.bloxd-io.com.az for free right in your browser. Build, compete, and explore the world in dynamic multiplayer mode with no downloads or installations required.
Football online https://qol.com.az/ goals, live match results, top scorers table, and detailed statistics. Follow the news and never miss the action.
pin up казино скачать на телефон бесплатно https://games-pinup.ru
Lily Phillips lilyphillips es te invita a un mundo de creatividad, conexion y emocionantes descubrimientos. Siguela en Instagram y Twitter para estar al tanto de nuevas publicaciones y proyectos inspiradores.
El sitio web oficial de Kareli Ruiz https://karelyruiz.es ofrece contenido exclusivo, noticias de ultima hora y actualizaciones periodicas. Mantengase al dia con las nuevas publicaciones y anuncios.
свадебное платье длинное каталог свадебных платьев купить цены
Нужны столбики? столбики для ограждения с лентами столбики для складов, парковок и общественных пространств. Прочные материалы, устойчивое основание и удобство перемещения обеспечивают безопасность и порядок.
купить кабель 6 кабель электрический купить минск