Juvenile Diabetes Explained: How It’s Different from Type 2 and What Every Parent Should Know
Contents
- 1 Juvenile Diabetes Explained: How It’s Different from Type 2 and What Every Parent Should Know
- 1.0.0.0.0.1 Read DISCLAIMER
- 1.0.0.0.0.2 The material presented here is for general informational and educational purposes only and is not medical advice. Although we attempt to provide current and accurate information, this blog should not be used as a replacement for professional medical consultation, diagnosis, or treatment. In all cases, consult your physician or an accredited medical practitioner with regards to any medical condition or treatment. Do not ignore professional medical advice or wait for it on the basis of information provided by this blog. In a medical emergency, call emergency services immediately.
- 1.1 Introduction: Beyond Labels—Understanding the Stories Behind Juvenile Diabetes
- 1.2 What Is Juvenile Diabetes—Really?
- 1.3 How Type 2 Diabetes Charts a Different Course
- 1.4 Onset Speed and Symptoms: A Tale of Two Journeys
- 1.5 Emotional Impact: How Diagnosis Shapes Lives Differently
- 1.6 Managing Care: Insulin vs. Lifestyle Shifts
- 1.7 Long-Term Risk and Complications
- 1.8 Real Life: What Families Often Overlook
- 1.9 Preventive Insights for Parents and Caregivers
- 1.10 Final Thoughts: Juvenile Diabetes Is Unique—But So Is Resilience
- 1.11 FAQs with Answers
Learn what juvenile diabetes (type 1) really is, how it differs from type 2, and what symptoms parents need to recognize early for proper care.
Read DISCLAIMER
The material presented here is for general informational and educational purposes only and is not medical advice. Although we attempt to provide current and accurate information, this blog should not be used as a replacement for professional medical consultation, diagnosis, or treatment. In all cases, consult your physician or an accredited medical practitioner with regards to any medical condition or treatment. Do not ignore professional medical advice or wait for it on the basis of information provided by this blog. In a medical emergency, call emergency services immediately.
Introduction: Beyond Labels—Understanding the Stories Behind Juvenile Diabetes
Juvenile diabetes isn’t just a medical term—it’s a life chapter that begins with questions like “Why is my child suddenly so thirsty?” or “Why are they losing weight despite eating more?” This condition, more formally known as type 1 diabetes, often starts abruptly, reshaping family routines and emotions. In contrast, type 2 diabetes develops gradually and is deeply tied to insulin resistance. By understanding how juvenile diabetes differs from type 2, caregivers gain clarity—and children gain care that honors who they are.

What Is Juvenile Diabetes—Really?
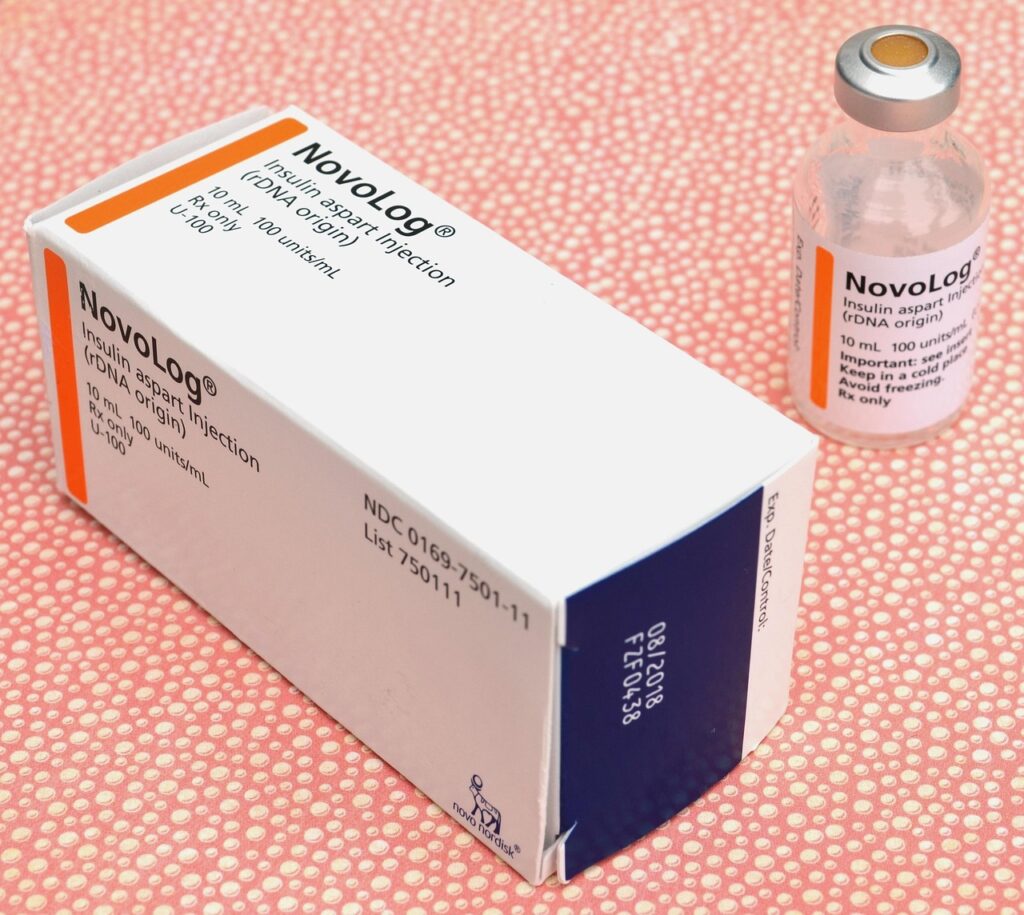
At its core, juvenile diabetes (type 1) happens when the immune system mistakenly attacks the beta cells in the pancreas that produce insulin. Without insulin, the body can’t move glucose from the bloodstream into cells, causing sugar to build up. It’s often referred to as insulin-dependent diabetes, because the body must rely entirely on external insulin. Diagnosis is sudden, with symptoms like thirst, fatigue, weight loss, and frequent urination arriving rapidly.
How Type 2 Diabetes Charts a Different Course
By contrast, type 2 diabetes usually begins with insulin resistance: the body produces insulin, but cells don’t respond well. The pancreas compensates until it can’t keep up, and blood sugar starts to rise. This progression occurs slowly, often tied to genetics, excess weight, diet, and inactivity. Unlike juvenile diabetes, onset can happen at any age—even in teens—but doesn’t always require immediate insulin.
Onset Speed and Symptoms: A Tale of Two Journeys
In juvenile diabetes, symptoms escalate quickly—sometimes over days. One moment your child is energetic; the next, they’re weak, thirsty, and losing weight. For parents, it can feel sudden and alarming. In type 2, subtle signs—slight fatigue, difficulty losing weight, mild thirst—emerge slowly over months or years, making detection more challenging and often overlooked until complications appear.
Emotional Impact: How Diagnosis Shapes Lives Differently
A juvenile diabetes diagnosis often brings shock, tears, and a steep learning curve—all at once. Insulin injections, carbohydrate counting, and blood sugar checks become daily rhythms. It’s a steep emotional adjustment for families. In type 2, sometimes people live with mild symptoms for years before noticing health impacts—it often feels less dramatic, but managing weight, diet, and exercise remains emotionally taxing in its own way.
Managing Care: Insulin vs. Lifestyle Shifts
Juvenile diabetes always requires insulin. Treatment focuses on balancing insulin with eating, activities, and growth. Care plans are precise. In type 2 diabetes, many people can begin with lifestyle changes—fiber-rich eating, movement, stress management—and may later use medications or insulin if needed. Both require monitoring glucose, but type 2 often offers more flexible options.
Long-Term Risk and Complications
In both forms, uncontrolled blood sugar can lead to health issues—but the timelines and risks differ. Juvenile diabetes may cause acute complications early on if not managed (like diabetic ketoacidosis), and long-term risks—heart or kidney issues—can appear if blood sugar stays elevated. In type 2, risk evolves over time, often tied to metabolic syndrome, weight, and insulin resistance. Both conditions benefit from early control and consistent care.
Real Life: What Families Often Overlook
Parents may dismiss early juvenile diabetes signs as “too busy” or “just growing pains.” Weight loss paired with increased thirst—especially in active children—can slip under the radar. When fatigue is written off as emotional or developmental, precious time may be lost. Many families tell me hindsight brought clarity—and relief. Early signs often whisper before they become loud.
Preventive Insights for Parents and Caregivers
Understanding both types of diabetes widens perspective. Type 1 arises unexpectedly. Type 2 reflects diet, activity, and genetic foundations. Optimizing nutrition, encouraging movement, and monitoring symptoms becomes vital—even for children. It’s not about blame—it’s about informed choices and early opportunities to cultivate health and strength.
Final Thoughts: Juvenile Diabetes Is Unique—But So Is Resilience
Juvenile diabetes may begin abruptly, but it doesn’t define a child’s joy, potential, or life. Distinguishing it from type 2 helps families respond accurately, supporting health and reducing fear. With insulin, awareness, community support, and compassionate care, children live vibrantly. And type 2, when diagnosed early, can often be managed or delayed. Understanding the differences is less about labels and more about empowering informed choices and thriving futures.
FAQs with Answers
- What is juvenile diabetes?
Juvenile diabetes, also known as type 1 diabetes, is an autoimmune condition where the body’s immune system destroys insulin-producing cells in the pancreas. Without insulin, glucose cannot enter cells, leading to high blood sugar and requiring lifelong insulin therapy for survival. - How does juvenile diabetes differ from type 2 diabetes?
The key difference is causation and age of onset. Juvenile diabetes develops suddenly in children due to immune-system targeting of pancreatic cells. It always requires insulin from diagnosis. Type 2 often develops later and gradually, often linked to insulin resistance, and may be managed through lifestyle changes or medications. - What symptoms typically appear in children with type 1 diabetes?
Children with juvenile diabetes often experience extreme thirst, frequent urination, rapid weight loss, and unexplained fatigue. These symptoms appear quickly—often over days—because the body can no longer regulate blood sugar without insulin. - Is juvenile diabetes only found in very young children?
While it’s called juvenile diabetes, type 1 can develop at any age—though it is most often diagnosed in childhood or adolescence. Diagnosis can happen in toddlers, pre-teens, or even early adults with a rapid-onset pattern. - Can a child with juvenile diabetes manage without insulin?
No. Juvenile diabetes is insulin-dependent from the moment of diagnosis. Without external insulin therapy, cells cannot use glucose for energy, which can lead to dangerous complications such as diabetic ketoacidosis. - What causes type 2 diabetes in younger people?
When children develop type 2, it often results from a combination of insulin resistance, excess weight, poor diet, and genetic susceptibility. It progresses slowly and may not require insulin initially, but it can worsen over time without intervention. - Can type 1 and type 2 symptoms in children overlap?
Yes. Symptoms like fatigue, thirst, hunger, and weight changes can appear in both types. However, type 1 symptoms often emerge suddenly and intensely, while type 2 usually develops more gradually over months or years. - How are type 1 and type 2 diabetes diagnosed differently in kids?
Diagnosis for juvenile diabetes often includes tests for autoantibodies and C‑peptide levels, which indicate immune attack on the pancreas. Type 2 diagnosis focuses on insulin resistance markers, fasting glucose trends, and assessments of family and lifestyle risk factors. - Can juvenile diabetes be prevented?
Currently, there is no known prevention for juvenile diabetes. It is an autoimmune condition with genetic influences. Research continues, but prevention remains elusive. Early detection and care management remain the priority. - What emotional impact can juvenile diabetes have on a child?
Children diagnosed with juvenile diabetes may feel anxious about injections or dietary restrictions. It can affect self-esteem or social interactions. Emotional support, open communication, and reassurance help children adapt and feel confident managing their condition. - Are complications different between type 1 and type 2 in children?
The complications can be similar—such as risk to kidneys, nerves, and heart—if blood sugar remains unmanaged. However, type 1 often carries earlier risk of diabetic ketoacidosis, and long-term care includes insulin management from the start. - How can parents support children newly diagnosed with juvenile diabetes?
Parents can support by learning insulin administration, carbohydrate counting, and glucose monitoring. Emotional validation, routine, and community support groups help rebuild confidence and reduce stress for both child and family. - Can children with type 2 diabetes avoid insulin?
Sometimes. If diagnosed early and managed with lifestyle changes—healthy nutrition, movement, weight management—a child with type 2 diabetes can maintain blood sugar control without insulin initially. - Are there different dietary approaches for juvenile diabetes vs type 2 in children?
Both types benefit from balanced nutrition, but juvenile diabetes requires precise carbohydrate counting and insulin timing. Type 2 management focuses on overall metabolic health, reducing refined carbs and increasing fiber and healthy fats. - Does exercise impact both types the same way?
Exercise improves insulin sensitivity and supports glucose balance in both types. For juvenile diabetes, careful timing relative to insulin dosing is essential to avoid low blood sugar. For type 2, movement often reduces insulin resistance and helps control weight and blood sugar.

Excellent read, I just passed this onto a friend who was doing some research on that. And he just bought me lunch because I found it for him smile So let me rephrase that: Thank you for lunch!
Nice post. I learn something more challenging on different blogs everyday. It will always be stimulating to read content from other writers and practice a little something from their store. I’d prefer to use some with the content on my blog whether you don’t mind. Natually I’ll give you a link on your web blog. Thanks for sharing.
**mindvault**
mindvault is a premium cognitive support formula created for adults 45+. It’s thoughtfully designed to help maintain clear thinking
**sugarmute**
sugarmute is a science-guided nutritional supplement created to help maintain balanced blood sugar while supporting steady energy and mental clarity.
**glpro**
glpro is a natural dietary supplement designed to promote balanced blood sugar levels and curb sugar cravings.
**vittaburn**
vittaburn is a liquid dietary supplement formulated to support healthy weight reduction by increasing metabolic rate, reducing hunger, and promoting fat loss.
**prodentim**
prodentim an advanced probiotic formulation designed to support exceptional oral hygiene while fortifying teeth and gums.
**glucore**
glucore is a nutritional supplement that is given to patients daily to assist in maintaining healthy blood sugar and metabolic rates.
**prostadine**
prostadine is a next-generation prostate support formula designed to help maintain, restore, and enhance optimal male prostate performance.
**sleep lean**
sleeplean is a US-trusted, naturally focused nighttime support formula that helps your body burn fat while you rest.
**synaptigen**
synaptigen is a next-generation brain support supplement that blends natural nootropics, adaptogens
**nitric boost**
nitric boost is a dietary formula crafted to enhance vitality and promote overall well-being.
**wildgut**
wildgutis a precision-crafted nutritional blend designed to nurture your dog’s digestive tract.
**mitolyn**
mitolyn a nature-inspired supplement crafted to elevate metabolic activity and support sustainable weight management.
**zencortex**
zencortex contains only the natural ingredients that are effective in supporting incredible hearing naturally.
**yu sleep**
yusleep is a gentle, nano-enhanced nightly blend designed to help you drift off quickly, stay asleep longer, and wake feeling clear.
**breathe**
breathe is a plant-powered tincture crafted to promote lung performance and enhance your breathing quality.
**pinealxt**
pinealxt is a revolutionary supplement that promotes proper pineal gland function and energy levels to support healthy body function.
**energeia**
energeia is the first and only recipe that targets the root cause of stubborn belly fat and Deadly visceral fat.
**prostabliss**
prostabliss is a carefully developed dietary formula aimed at nurturing prostate vitality and improving urinary comfort.
**boostaro**
boostaro is a specially crafted dietary supplement for men who want to elevate their overall health and vitality.
**potent stream**
potent stream is engineered to promote prostate well-being by counteracting the residue that can build up from hard-water minerals within the urinary tract.
**hepatoburn**
hepatoburn is a premium nutritional formula designed to enhance liver function, boost metabolism, and support natural fat breakdown.
**hepato burn**
hepato burn is a potent, plant-based formula created to promote optimal liver performance and naturally stimulate fat-burning mechanisms.
**flowforce max**
flowforce max delivers a forward-thinking, plant-focused way to support prostate health—while also helping maintain everyday energy, libido, and overall vitality.
**prodentim**
prodentim is a forward-thinking oral wellness blend crafted to nurture and maintain a balanced mouth microbiome.
**cellufend**
cellufend is a natural supplement developed to support balanced blood sugar levels through a blend of botanical extracts and essential nutrients.
**neurogenica**
neurogenica is a dietary supplement formulated to support nerve health and ease discomfort associated with neuropathy.
**revitag**
revitag is a daily skin-support formula created to promote a healthy complexion and visibly diminish the appearance of skin tags.
Alright, alright, 615betwin, eh? Giving it a shot! Seems legit so far. Let’s see if it lives up to the hype! Check it out: 615betwin
OkeBet Login – simple and straightforward, I hope! Ain’t nobody got time for complicated logins. Let’s get to the games! Hoping for some exciting spins! okebetlogin
Yo, 777kingvip is pretty sweet! Been playing there lately and gotta say, the slots are fire. Could use a few more promos, but other than that, it’s a solid spot. Definitely worth checking out if you’re looking for a new place to spin some reels. Check it out here: 777kingvip
**mitolyn reviews**
Mitolyn is a carefully developed, plant-based formula created to help support metabolic efficiency and encourage healthy, lasting weight management.