Can You Survive Brain‑Eating Amoeba? Explanation
Contents
- 1 Can You Survive Brain‑Eating Amoeba? Explanation
- 1.0.0.0.0.1 Read DISCLAIMER
- 1.0.0.0.0.2 The material presented here is for general informational and educational purposes only and is not medical advice. Although we attempt to provide current and accurate information, this blog should not be used as a replacement for professional medical consultation, diagnosis, or treatment. In all cases, consult your physician or an accredited medical practitioner with regards to any medical condition or treatment. Do not ignore professional medical advice or wait for it on the basis of information provided by this blog. In a medical emergency, call emergency services immediately.
- 1.1 Facing the Fear: Why This Topic Hits Home
- 1.2 What Happens When Naegleria fowleri Enters the Body
- 1.3 Recognizing the Critical Window for Action
- 1.4 What Makes Some People Survive?
- 1.5 The Emotional Journey of Survival
- 1.6 Why Treatment Is So Urgent and Complex
- 1.7 How Doctors Keep the Window Open
- 1.8 Can You Increase Your Survival Odds?
- 1.9 Research Into New Treatments and Diagnostics
- 1.10 Hope Through Awareness
- 1.11 Final Thoughts: Survival Is Not Fiction, But Not Common
- 1.12 FAQs with Answers
Can you survive a brain-eating amoeba? Discover the harsh realities of Naegleria fowleri, how it invades the brain, survival possibilities, treatment challenges, and the latest research on prevention and recovery.
Read DISCLAIMER
The material presented here is for general informational and educational purposes only and is not medical advice. Although we attempt to provide current and accurate information, this blog should not be used as a replacement for professional medical consultation, diagnosis, or treatment. In all cases, consult your physician or an accredited medical practitioner with regards to any medical condition or treatment. Do not ignore professional medical advice or wait for it on the basis of information provided by this blog. In a medical emergency, call emergency services immediately.
Facing the Fear: Why This Topic Hits Home
When people hear the term “brain‑eating amoeba,” panic can set in instantly. It sounds like a horror movie plot—and in many ways, it can feel that way. But the reality is far more complex: Naegleria fowleri is a microscopic organism rarely encountered, yet capable of causing Primary Amoebic Meningoencephalitis (PAM), a devastating brain infection. Survival is possible—but only in very rare cases. To understand how survival happens, or why so few people survive, we need to explore what the infection is like from start to finish, humanize the experience, and understand the science and treatment at play.
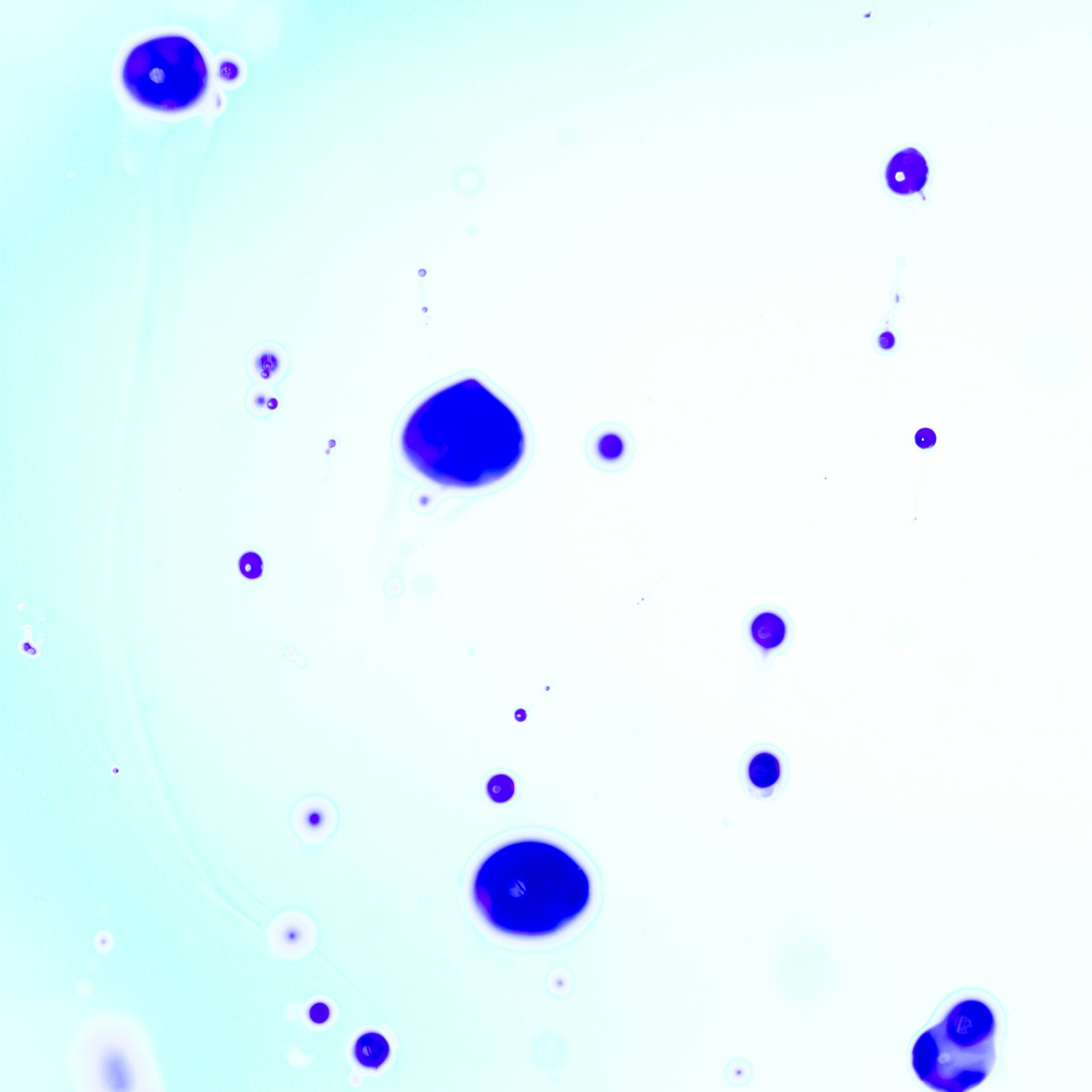
What Happens When Naegleria fowleri Enters the Body
The brain‑eating amoeba lives in warm freshwater and sometimes enters the body through the nose—during swimming, diving, or nasal rinsing with unsterile water. Once inside, it travels up the olfactory nerve and reaches the frontal lobe. The trophozoites multiply rapidly and release enzymes that break down brain tissue. At the same time, the immune system triggers inflammation, but in the enclosed cranial cavity, that inflammation contributes to brain swelling, pressure, and tissue damage. Symptoms begin with headache and fever and intensify in a matter of days. For most people, survival isn’t possible, but understanding why some do recover offers hope—and crucial learning.
Recognizing the Critical Window for Action
The hallmark of PAM is its rapid progression. Initial symptoms may resemble flu or viral meningitis. A headache starts suddenly, followed by fever, nausea, vomiting, and stiff neck. As the infection advances, confusion, hallucinations, seizures, and coma can follow. Death often occurs within 5 to 7 days.
But in the rare survivors, symptoms were recognized and treated within the first day or two. Those survivors formed the basis of our knowledge about effective treatment approaches. Recovery requires immediate awareness—of the symptoms, of the potential exposure, and of the need to push for aggressive diagnosis and intervention.
What Makes Some People Survive?
- Recognition of symptoms and timely medical attention—often within 48 hours of symptom onset.
- Immediate lumbar puncture and rapid testing of cerebrospinal fluid.
- Administration of amphotericin B, sometimes intrathecally, within hours of suspicion.
- Use of experimental treatments like miltefosine (an anti‑parasitic drug) in combination with other antifungals and antibiotics.
- Intensive supportive care: management of brain swelling, seizure control, hypothermia therapy, and continuous monitoring in an ICU.
Yet even with all this, only a handful of people worldwide have survived. Those who do often face long, difficult recoveries with neurological impairments.
The Emotional Journey of Survival
Imagine waking up thinking you have a headache. Within hours, you’re confused, delirious, unable to follow simple instructions. Your loved ones bring you to a hospital, but doctors don’t immediately suspect anything unusual. Then, someone notices a swim incident days ago. That’s often when the shift occurs—from dismissing symptoms as a migraine or flu, to a life‑and‑death medical battle.
Survivors who’ve shared their stories often speak of the fragility of life, the kindness of medical teams, and the emotional trauma. Recovery may involve relearning to walk, to speak, or to process thoughts. But surviving is possible—and each survivor provides key insights for medical science.
Why Treatment Is So Urgent and Complex
Inhibiting the amoeba requires aggressive drug therapy. Amphotericin B is the standard—but it has severe toxicity, and dosing must be carefully monitored. Miltefosine, used experimentally, has shown promise in a few cases. Steroids like dexamethasone may help control inflammation. Induced hypothermia can slow the metabolic destruction. Seizures must be managed. Brain pressure must be relieved. Every intervention risks side effects, but delaying treatment is far more dangerous.
How Doctors Keep the Window Open
Clinicians faced with suspected PAM need to act quickly. Once lumbar puncture confirms amoeba presence or PCR testing detects DNA, the treatment clock starts. The survivor stories all feature aggressive protocols: combination medications, neurosurgical decompression in some cases, hypothermia therapy, and expert ICU management.
Can You Increase Your Survival Odds?
The takeaway for individuals is:
- Be aware: Know the early symptoms, especially after freshwater exposure.
- Speak up: If symptoms follow possible exposure, demand testing.
- Push hard: Ask specifically for Naegleria testing if meningitis is suspected.
- Don’t delay: Early intervention is the only chance to survive.
Even then, survival is not guaranteed—but knowledge empowers.
Research Into New Treatments and Diagnostics
Researchers are actively studying genetic markers in survivors, immune system responses, and faster diagnostic tools like real-time PCR tests. New drugs are under investigation, and smarter immune modulation (to reduce inflammation without suppressing anti‑amoebic activity) is an area of ongoing exploration.
Animal studies, case review registries, and laboratory testing are slowly improving outcomes—but progress is challenging when the infection is rare and fatalities are fast.
Hope Through Awareness
Talking about PAM doesn’t have to sound doomsday. Instead, it can be framed as vigilance. Understanding how survival happens gives families, clinicians, and communities a fighting chance. And clinicians who’ve diagnosed PAM often describe their initial encounter as challenging—because they had to interpret symptoms quickly, advocate for lumbar puncture, and push for aggressive treatment even when typical outcomes seemed poor.
Final Thoughts: Survival Is Not Fiction, But Not Common
Yes, people can survive brain‑eating amoeba infection—but only in rare situations that include rapid identification and aggressive treatment. Every survivor has helped science learn more. But survival mostly depends on speed—of recognition, of testing, of treatment.
If you or someone you know develops sudden severe neurologic symptoms after any freshwater exposure, seek medical help immediately, mention the possibility, and advocate for testing. Survival may be rare—but it is possible.
FAQs with Answers
- What is a brain-eating amoeba?
It is a rare but deadly organism called Naegleria fowleri that enters the brain through the nose, causing a condition called Primary Amoebic Meningoencephalitis (PAM). - How does the amoeba enter the human body?
It usually enters through the nose when people swim or dive in warm freshwater lakes, rivers, or poorly maintained pools. - Can you survive brain-eating amoeba infection?
Survival is extremely rare, but possible with early diagnosis, aggressive treatment using amphotericin B, miltefosine, and supportive care. - What are the early symptoms?
Fever, headache, nausea, stiff neck, and confusion are early signs. Symptoms appear within 1 to 12 days of exposure. - How quickly does the infection progress?
It progresses rapidly, often leading to death within 5 to 7 days after symptom onset. - Why is it called “brain-eating”?
Because Naegleria fowleri destroys brain tissue as it multiplies, causing severe inflammation and death. - Is it contagious from person to person?
No, it does not spread through person-to-person contact or by drinking contaminated water. - Where is this amoeba found?
In warm freshwater environments such as lakes, rivers, hot springs, and unchlorinated swimming pools. - What increases the risk of infection?
Activities like diving, water sports, using neti pots with unboiled tap water, and swimming in warm, stagnant freshwater increase the risk. - Can chlorine kill the amoeba?
Yes, proper chlorination of pools and water systems can kill the amoeba and prevent infection. - Are children more at risk?
Children and young adults are more likely to engage in water activities that increase the risk of nasal exposure. - Can it be diagnosed early?
Early diagnosis is difficult due to symptom similarity with meningitis, but advanced lab tests and awareness can improve outcomes. - What is the current treatment?
A combination of antifungal drugs like amphotericin B, rifampin, azithromycin, and miltefosine, along with supportive ICU care. - What’s the survival rate?
Historically, over 97% of diagnosed cases have been fatal, with only a few documented survivors worldwide. - How can I protect myself?
Avoid freshwater exposure during high temperatures, use nose clips, avoid stirring up sediment, and don’t use tap water in nasal rinses unless boiled or filtered.
Hey I know this is off topic but I was wondering if you knew of any widgetsI could add to my blog that automatically tweet my newest twitter updates. http://www.kayswell.com
Very interesting subject , thankyou for posting.
Hello my loved one! I wish to say that this post is amazing, great written and include approximately all significant infos. I would like to peer extra posts like this . http://www.kayswell.com
Generally I don’t read article on blogs, but I wish to say that this write-up very forced me to try and do so! Your writing style has been surprised me. Thanks, quite nice article.
I have not checked in here for a while since I thought it was getting boring, but the last several posts are great quality so I guess I will add you back to my everyday bloglist. You deserve it my friend 🙂
Entdecken Sie die besten Weinverkostungen in Wien auf weinverkostung in wien.
Die osterreichische Hauptstadt bietet eine einzigartige Mischung aus Tradition und Moderne.
Die Weinverkostungen in Wien sind perfekt fur Kenner und Neulinge. Zusatzlich gibt es oft kulinarische Begleitungen, die den Genuss erhohen.
#### **2. Die besten Orte fur Weinverkostungen**
In Wien gibt es zahlreiche Lokale und Weinguter, die Verkostungen anbieten. Auch moderne Weinkeller in der Innenstadt bieten exklusive Erlebnisse.
Einige Winzer veranstalten Fuhrungen durch ihre Kellereien. Zusatzlich konnen Gaste direkt beim Erzeuger kosten.
#### **3. Wiener Weinsorten und ihre Besonderheiten**
Wiener Weine sind vor allem fur ihre Vielfalt bekannt. Auch der fruchtige Grune Veltliner zahlt zu den bekanntesten Wei?weinen der Region.
Die Bodenbeschaffenheit und das Klima pragen den Geschmack. Die mineralischen Noten der Wiener Weine sind besonders ausgepragt.
#### **4. Tipps fur eine gelungene Weinverkostung**
Eine gute Vorbereitung macht die Verkostung noch angenehmer. Ein neutraler Geschmack im Mund vor der Verkostung verbessert das Erlebnis.
Gruppenverkostungen bringen zusatzlichen Spa?. Viele Veranstalter bieten thematische Verkostungen an.
—
### **Spin-Template fur den Artikel**
#### **1. Einfuhrung in die Weinverkostung in Wien**
Viele Veranstaltungen werden von erfahrenen Sommeliers begleitet.
#### **2. Die besten Orte fur Weinverkostungen**
Das bekannte Heurigenviertel in Grinzing ladt zu gemutlichen Verkostungen ein.
#### **3. Wiener Weinsorten und ihre Besonderheiten**
Auch der fruchtige Grune Veltliner zahlt zu den bekanntesten Wei?weinen der Region.
#### **4. Tipps fur eine gelungene Weinverkostung**
Gemeinsames Diskutieren uber die Aromen fordert den Austausch.
Discover exquisite Austrian wines at wine-tasting-wien.netlify.app and immerse yourself in Vienna’s vibrant wine culture.
Die osterreichische Hauptstadt bietet eine einzigartige Mischung aus Tradition und Moderne. Die Region ist bekannt fur ihren exzellenten Wei?wein, besonders den Grunen Veltliner. Viele Weinverkostungen finden in historischen Gewolbekellern statt.
Das milde Klima und die mineralreichen Boden begunstigen den Weinbau. Daher gedeihen hier besonders aromatische Rebsorten.
#### **2. Beliebte Weinregionen und Weinguter**
In Wien gibt es mehrere renommierte Weinregionen, wie den Nussberg oder den Bisamberg. Diese Gebiete sind fur ihre Spitzenweine international bekannt. Familiengefuhrte Weinguter bieten oft Fuhrungen und Verkostungen an. Dabei lernt man viel uber die Herstellung und Geschichte der Weine.
Ein Besuch im Weingut Wieninger oder im Mayer am Pfarrplatz lohnt sich. Hier verbinden sich Tradition mit innovativen Methoden.
#### **3. Ablauf einer typischen Weinverkostung**
Eine klassische Wiener Weinverkostung beginnt meist mit einer Kellertour. Die Winzer erklaren gerne ihre Arbeitsschritte. Danach folgt die Verkostung unterschiedlicher Weine. Die Aromen werden von den Experten detailliert beschrieben.
Haufig werden die Weine mit lokalen Kasesorten oder Brot serviert. Diese Kombination ist ein Highlight fur Feinschmecker.
#### **4. Tipps fur unvergessliche Weinverkostungen**
Um das Beste aus einer Weinverkostung in Wien herauszuholen, sollte man vorher buchen. Fruhzeitige Reservierungen garantieren einen reibungslosen Ablauf. Zudem lohnt es sich, auf die Jahreszeiten zu achten. Die warmen Monate eignen sich perfekt fur Verkostungen im Freien.
Ein guter Tipp ist auch, ein Notizbuch mitzubringen. So kann man sich die geschmacklichen Eindrucke leicht merken.
—
### **Spin-Template fur den Artikel**
#### **1. Einfuhrung in die Weinverkostung in Wien**
Daher gedeihen hier besonders aromatische Rebsorten.
#### **2. Beliebte Weinregionen und Weinguter**
Sie sind bekannt fur ihre ausgezeichneten Jahrgange.
#### **3. Ablauf einer typischen Wiener Weinverkostung**
Das unterstreicht die Geschmacksnuancen der Weine.
#### **4. Tipps fur unvergessliche Weinverkostungen**
Im Winter bieten viele Weinguter gemutliche Kellerveranstaltungen.
—
**Hinweis:** Durch Kombination der Varianten aus den -Blocken konnen zahlreiche einzigartige Texte generiert werden, die grammatikalisch und inhaltlich korrekt sind.
vavada casino pl
Nabycie nieruchomosci w Beskidach to szansa na stworzenie wymarzonego miejsca na wakacje lub staly dom.
Dzieki rozwijajacej sie infrastrukturze i rosnacemu zainteresowaniu turystow, ceny dzialek stopniowo wzrastaja. Coraz wiecej osob docenia spokoj i piekno przyrody, jakie oferuja Beskidy.
#### **2. Gdzie szukac najlepszych ofert dzialek?**
Wybor odpowiedniej lokalizacji zalezy od indywidualnych potrzeb i budzetu. Najlepsze propozycje mozna znalezc na specjalistycznych serwisach, gdzie dostepne sa dzialki o roznej powierzchni i standardzie.
Przed zakupem nalezy dokladnie przeanalizowac dostepnosc mediow i warunki zabudowy. Wiele ofert zawiera szczegolowe informacje o mozliwosciach zagospodarowania terenu, co ulatwia podjecie decyzji.
#### **3. Jakie korzysci daje posiadanie dzialki w Beskidach?**
Nieruchomosc w gorach to nie tylko inwestycja finansowa, ale rowniez szansa na poprawe jakosci zycia. Dzialka w Beskidach moze stac sie zrodlem dochodu, jesli zdecydujemy sie na wynajem turystom.
Dodatkowo, region ten oferuje wiele atrakcji, takich jak szlaki turystyczne i stoki narciarskie. Wlasciciele dzialek moga korzystac z licznych festiwali i wydarzen kulturalnych organizowanych w regionie.
#### **4. Jak przygotowac sie do zakupu dzialki?**
Przed podjeciem decyzji warto skonsultowac sie z prawnikiem i geodeta. Profesjonalna pomoc pozwoli uniknac nieprzyjemnych niespodzianek zwiazanych z formalnosciami.
Wazne jest rowniez okreslenie swojego budzetu i planow zwiazanych z zagospodarowaniem terenu. Warto rozwazyc wszystkie opcje, aby wybrac najlepsza dla siebie mozliwosc.
—
### **Szablon Spinu**
**1. Dlaczego warto kupic dzialke w Beskidach?**
– Beskidy to idealne miejsce dla osob szukajacych spokoju i bliskosci natury.
– Rosnaca popularnosc tego regionu przeklada sie na wzrost wartosci nieruchomosci.
**2. Gdzie szukac najlepszych ofert dzialek?**
– Warto przegladac specjalistyczne portale, ktore skupiaja sie na nieruchomosciach w Beskidach.
– Kluczowe jest sprawdzenie, czy dzialka ma wszystkie niezbedne pozwolenia.
**3. Jakie korzysci daje posiadanie dzialki w Beskidach?**
– Dzialka w Beskidach moze stac sie zrodlem dodatkowego dochodu dzieki wynajmowaniu turystom.
– Wlasciciele dzialek moga uczestniczyc w lokalnych wydarzeniach i festiwalach.
**4. Jak przygotowac sie do zakupu dzialki?**
– Konsultacja z geodeta pomoze uniknac problemow z granicami nieruchomosci.
– Rozmowa z dotychczasowymi wlascicielami moze dostarczyc cennych informacji.
производства натяжных потолков
Они отличаются практичностью и долговечностью.
Компания “natyazhni-steli-vid-virobnika.biz.ua” предлагает качественные потолки напрямую от производителя. Клиенты получают гарантированно надежные решения.
#### **2. Преимущества натяжных потолков**
Одним из главных плюсов натяжных потолков является их влагостойкость. Даже при затоплении потолок останется целым.
Еще одно преимущество — огромный выбор цветов и фактур. Вы можете подобрать глянцевую, матовую или сатиновую поверхность.
#### **3. Производство и материалы**
Наша компания изготавливает потолки из экологически чистого ПВХ. Он не выделяет вредных веществ даже при нагревании.
Технология производства гарантирует прочность и эластичность полотна. Каждое полотно проходит проверку перед отправкой клиенту.
#### **4. Установка и обслуживание**
Монтаж натяжных потолков занимает всего несколько часов. Уже через день вы сможете пользоваться обновленным помещением.
Уход за потолком не требует особых усилий. Пятна и пыль легко удаляются без специальных средств.
—
### **Спин-шаблон статьи**
#### **1. Введение**
Натяжные потолки — это стильное и удобное решение для любого дома.
#### **2. Преимущества натяжных потолков**
Натяжные конструкции исключают риск появления трещин и провисаний.
#### **3. Производство и материалы**
Готовые потолки сохраняют форму десятилетиями благодаря особой технологии.
#### **4. Установка и обслуживание**
Легкая влажная уборка поможет поддерживать потолок в идеальном состоянии.
I enjoy, cause I discovered just what I was having a look for. You’ve ended my four day lengthy hunt! God Bless you man. Have a nice day. Bye
You have brought up a very great details, appreciate it for the post.
I tried out TP88vn a little while ago. The website is modern looking, games are good. Overall, nothing too crazy, but it’s reliable and fun. Check ’em out: tp88vn
Dead composed content, Really enjoyed looking through.
You could certainly see your skills in the work you write. The world hopes for even more passionate writers like you who are not afraid to say how they believe. Always follow your heart.
Excellent post. I was checking continuously this blog and I am impressed! Very useful info particularly the last part 🙂 I care for such information a lot. I was looking for this particular information for a very long time. Thank you and best of luck.
I like this website very much, Its a very nice position to read and incur information.
Trying to get logged into jili711login. Hope it’s smooth and easy. Ready to play some games! Wish me luck people because I am going to need it. Visit them now jili711login!
VN88cuoc, been hearing good things. Seems to have a lot of active players, so that’s a good sign. Time to get in the action and see what all the fuss is about. vn88cuoc
Hey there, You’ve done a great job. I’ll definitely digg it and personally suggest to my friends.
I am confident they will be benefited from this website.
I think other web site proprietors should take this website as an model, very clean and fantastic user friendly style and design, as well as the content. You’re an expert in this topic!
Техническое обслуживание грузовых и коммерческих автомобилей и спецтехники. Снабжение и поставки комплектующих для грузовых автомобилей, легкового коммерческого транспорта на бортовой платформе ВИС lada: https://ukinvest02.ru/
Для детской лучше брать безопасные материалы и заранее продумать свет и вентиляцию, выбирайте бесшовная ткань, оно не требует ежегодной покраски и обновления, попросите образцы при дневном и теплым вечерним светом, вы сохраните нервы и не будете переделывать потолок через год: https://natyazhnye-potolki-moskva.ru/
https://sonabet.pro/
Натяжной потолок упрощает уход и экономит время на уборке, оформляют монтаж в компании Потолки Москвы, хорошо переносит перепады температуры в квартире; подбирают профиль и аккуратные вставки, Такой потолок легко вписать в минимализм и классику – https://potolki-decarat.ru/
If you need a reliable way to get around the city, renting a car in Auckland is often the easiest option. There are different vehicle classes, airport pickups, and flexible rental periods available: Auckland car rental
Как рассчитать проценты за пользование чужими средствами по статье 395 ГК РФ – быстро, просто и без ошибок. Смотрите, какую инструкцию можно использовать и какой онлайн-калькулятор поможет сэкономить время https://voronezh-tsk.ru/stati/raschet-protsentov-po-395-gk-rf/
На big-bag-rus.ru вы можете купить биг-бэги и мягкие контейнеры МКР от производителя: мешки биг бэги 1–4 стропы, с верхней сборкой, люками и вкладышем. Изготовление под ваши требования, стабильное качество, выгодный опт и отгрузка по России: https://big-bag-rus.ru/
You have observed very interesting points! ps nice site. “Never take the advice of someone who has not had your kind of trouble.” by Sydney J. Harris.
Купить рефералов Blum: ТОП лучших сервисов и бесплатные методы https://vc.ru/1250655
https://pamyatniki-granitnye.by/
сайт с закладками https://memori.ru/
Деньги в долг в Казахстане можно получить онлайн. Не требуется личное посещение офиса. Процесс оформления понятен. Решение принимается быстро. Деньги перечисляются удобным способом – кредит наличными казахстан
Electric roadsters are sporty, two-seat electric cars designed for fast acceleration and open-top driving. They focus on performance, style, and driving excitement https://ev.motorwatt.com/ev-manufacturers/
Живая накрутка ТГ канал – ТОП-27 способов в 2026 году. Наш рейтинг https://vc.ru/1549490
https://indwin-app-7-india.com/
7k casino предоставляет доступ к актуальным онлайн играм. Каталог регулярно обновляется. Пользователь может выбирать подходящий формат. Сайт работает стабильно. Это поддерживает интерес: 7к казино сайт
reefer dispatch service
7k casino предлагает удобную онлайн среду для игры. Все функции доступны через личный кабинет. Пользователь контролирует игровой процесс. Навигация проста. Это делает использование комфортным: 7к казино сайт
Долфин Анти: https://долфин-анти.рф/ Современный антидетект-браузер для безопасного управления множеством аккаунтов. Эффективное решение для арбитража трафика, криптопроектов и автоматизации маркетинга без риска блокировок.
https://l1l.kz/5eR7s4
https://mhp.ooo/
Avia Masters de BGaming es un juego crash con RTP del 97% donde apuestas desde 0,10€ hasta 1.000€, controlas la velocidad de vuelo de un avion que recoge multiplicadores (hasta x250) mientras evita cohetes que reducen ganancias a la mitad, con el objetivo de aterrizar exitosamente en un portaaviones para cobrar el premio acumulado
feg.org.es
Avia Masters de BGaming es un juego crash con RTP del 97% donde apuestas desde 0,10€ hasta 1.000€, controlas la velocidad de vuelo de un avion que recoge multiplicadores (hasta x250) mientras evita cohetes que reducen ganancias a la mitad, con el objetivo de aterrizar exitosamente en un portaaviones para cobrar el premio acumulado
https://share.google/6NZqG87EYSokcLBlY
What’s up Dear, are you actually visiting this web page
daily, if so afterward you will without doubt take pleasant knowledge.
ко ланта ко ланта
Hi there to all, how is the whole thing, I think every one is getting more from this web page, and your views are fastidious for new viewers.
byueuropaviagraonline
дешевые цветы москва Быстро розы сюрприз доставка
Ahaa, its fastidious dialogue on the topic of this paragraph at this place at this weblog, I
have read all that, so now me also commenting here.
замена замков Квалифицированный ремонт замков всех типов. Продлите жизнь вашему замку!
краби таиланд как добраться с аэропорта пхукета до краби
https://auto.qa/catalog/
тикток мод тг тик ток мод 2026 года бесплатно
рунетки чат рунетки онлайн
https://jasonejohnson11.blogspot.com/2026/01/elevate-your-homes-comfort-with-gas.html We spent time on a long process researching a gas fireplace for a home upgrade, and what was most noticeable was how various brands handle heat output and installation details. Certain models focus primarily on visual appeal, while others put more emphasis on efficiency. It was helpful to compare venting options, control systems, and long-term maintenance requirements before making a decision. If someone is considering a similar project, it’s worth spending time learning how gas fireplaces actually perform during regular use, not just how they appear in marketing images.
хочу поехать в корею работать работа в корее отзывы девушек
Your mode of describing the whole thing in this article is
truly good, every one be capable of simply be aware of it, Thanks a lot.
рунетки рунетки чат
Зеркало поворотное большое Трюмо с тремя зеркалами: идеальное решение для создания макияжа и причесок с разных ракурсов.
Военная служба по договору отличается прозрачными условиями. Выплаты начисляются официально. Контракт заключается на определенный срок. Возможна пролонгация – военнослужащий по контракту вакансии спб
La esencia fundamental de AviaMasters es su sistema de vuelo dinГЎmico. Distinto de la mayorГa de juegos de crash, aquГ no solo miras, sino que tambiГ©n sientes la adrenalina constante de cada movimiento estratГ©gica.
aviamasters.nom.es
https://rant.li/larrybrown190/revamp-your-kitchen-for-a-cozy-and-functional-space
While looking into space heaters, I noticed that Comfort Glow heaters are often mentioned in discussions about basic efficiency and safety features. For compact spaces or supplemental heating, those factors tend to be more important than raw power.
Looking at various heater manufacturers helped me understand how air circulation, temperature control, and safety mechanisms affect everyday comfort. It’s not always about the highest heat level, but about steady performance and safe operation over time.
Кент казино ориентировано на современный онлайн формат. Платформа поддерживает разные устройства. Игры корректно работают на смартфонах и ПК. Интерфейс адаптивный. Пользователь легко осваивается: кент казино промокод
https://community.hodinkee.com/members/xbetfreecode
пошив штор на заказ Шторы на заказ – это возможность создать уникальный элемент декора, идеально соответствующий вашим требованиям и предпочтениям. Выбор ткани, фактуры, цвета и декоративных элементов позволяет подчеркнуть особенности интерьера и создать неповторимую атмосферу.
https://bridesofbakewell.com/pages/888starz_promo_code____vip_bonus_.html
Казино Atom это современный онлайн формат азартных игр. Удобный вход и рабочее зеркало всегда доступны. Бонус казино Atom позволяет начать выгодно. Заходи сейчас – atom казино официальный сайт
https://mitsubishi-climate.ru/images/pgs/promokod_fonbet_bonus_2.html
https://pechi-sauna.ru/wp-content/pgs/1xbet_promokod_besplatno_bonus.html
https://redclara.net/news/pgs/?code_promo_melbet_pour_l_inscription.html
1xbet registration promo code singapore
упаковка оптом Упаковка на заказ – это проявление индивидуальности, возможность выделиться на фоне конкурентов и подчеркнуть уникальность своего бренда. Разработка дизайна, выбор материалов и контроль качества на каждом этапе производства – все это направлено на создание упаковки, которая будет соответствовать вашим самым высоким требованиям.
https://dogs-academia.ru/
https://service-trucks.ru/
Если важен быстрый старт и бонусы выбирай куш казино официальный сайт. Удобный вход и понятный интерфейс. Регистрация не занимает много времени. Заходи и пробуй удачу – казино куш зеркало
https://svobodapress.com.ua/pryvitannia-z-45-richchiam-cholovikovi-u-virshakh-naykrashchi-virshi-ta-pobazhannia/
1xbet promo code free spins egypt
Cactus casino официальный сайт выбирают за надежность и удобство. Быстрый вход и простая регистрация. Бонусы доступны сразу. Присоединяйся к игре – cactus casino вход
Общество экспертов России по недропользованию – профессиональный портал для оценки статуса и компетенций экспертов по экспертизе недр. Ресурс упрощает подобрать специалиста по профилям: нефть и газ, геология и ГРР, ТПИ – и снизить риски при согласовании отчетов и отчетов в сделках: https://oern2007.ru/
Индивидуалки Сургута
https://t.me/sex_vladivostoka
https://t.me/nur_intim
Продам револейд Продам Рисарг. Препарат для лечения гипертонии.
Металлические стеллажные системы промышленного назначения изготавливаются с учетом нормативных требований и условий эксплуатации. Мы используем расчет нагрузок и инженерное проектирование. Производство ориентировано на надежность и долговечность. Такие решения подходят для интенсивной работы склада – паллетные фронтальные стеллажи
розыгрыши ключей ключи steam
Кент казино вход реализован с учётом удобства и скорости. Пользователь может быстро авторизоваться и перейти к игре. Процесс не отвлекает от основного – kent casino зеркало
Kasyno Vavada przyciaga graczy licencja Curacao oraz codziennymi bonusami bez depozytu.
Po szybkiej rejestracji kod promocyjny daje darmowe spiny na topowych slotach z wysokim RTP.
Turnieje z pula nagrod i rankingami motywuja do aktywnej gry, a blyskawiczne wyplaty buduja zaufanie.
Aktualne lustra omijaja blokady, wiec dostep do konta pozostaje stabilny 24/7.
Sprawdz najnowsze promocje i instrukcje aktywacji kodu tutaj: https://utahmixedmartialartstraining.com/.
Graj odpowiedzialnie i ustaw limity bankrolu, aby rozrywka pozostala bezpieczna.
Онлайн платформа 7k casino предлагает игрокам гибкий выбор игр и форматов. Это позволяет подобрать оптимальный стиль игры под личные предпочтения: 7k casino сайт регистрация
цветы момент
Kasyno Vavada regularnie aktualizuje kody bonusowe, oferujac darmowe spiny oraz premie bez depozytu.
Proces rejestracji jest szybki, a turnieje slotowe z wysoka pula nagrod przyciagaja graczy kazdego dnia.
Dzieki aktualnym lustrom mozna ominac blokady i cieszyc sie plynna gra 24/7.
Nowe promocje oraz instrukcje wyplat znajdziesz tutaj: vavada kontakt.
Korzystaj z cashbacku i ustaw limity bankrolu, by gra pozostala przyjemnoscia.
Мы верим, что каждая женщина заслуживает качественной информации и вдохновения. Поэтому в нашем журнале вы найдёте статьи о красоте, здоровье, детях и семейных отношениях. Переходите по ссылке и оставайтесь с нами https://universewomen.ru/
Шоурумы столицы привлекают не только жителей города, но и гостей Москвы, которые хотят познакомиться с локальными брендами. Такой формат помогает открыть новые имена в модной индустрии. Это расширяет возможности для выбора. Узнать больше можно по ссылке: https://forextema.com/index.php?option=com_easyblog&view=entry&id=14407&Itemid=75
What i do not realize is actually how you’re now not actually a lot more smartly-preferred than you may be now.
You are so intelligent. You already know thus significantly with regards
to this subject, produced me personally consider
it from a lot of various angles. Its like women and men aren’t fascinated unless it’s one thing to accomplish with Girl gaga!
Your individual stuffs great. Always take care of it up!
I am regular reader, how are you everybody? This piece of writing
posted at this web page is truly good.
сайт заказа цветов
Гвоздики в классических композициях купите
Шоурумы Москвы привлекают тех, кто устал от массового рынка и хочет подчеркнуть индивидуальность. Здесь представлены лимитированные коллекции, авторские бренды и качественные ткани. Такой формат позволяет делать осознанный выбор и инвестировать в стиль, http://rossbiz.ru/home/414581