A Gentle Introduction: Understanding Type 1 and Type 2 Diabetes With Clarity, Compassion, and Calm
Contents
- 1 A Gentle Introduction: Understanding Type 1 and Type 2 Diabetes With Clarity, Compassion, and Calm
- 1.0.0.0.0.1 Read DISCLAIMER
- 1.0.0.0.0.2 The material presented here is for general informational and educational purposes only and is not medical advice. Although we attempt to provide current and accurate information, this blog should not be used as a replacement for professional medical consultation, diagnosis, or treatment. In all cases, consult your physician or an accredited medical practitioner with regards to any medical condition or treatment. Do not ignore professional medical advice or wait for it on the basis of information provided by this blog. In a medical emergency, call emergency services immediately.
- 1.1 Why Learning the Difference Matters More Than Most People Realize
- 1.2 What Diabetes Really Means: Understanding the Foundation Before Exploring the Differences
- 1.3 The Emotional Weight of the Diagnosis and Why Understanding Brings Relief
- 1.4 Why Comparing Type 1 and Type 2 Diabetes Can Be Confusing Without a Clear Framework
- 1.5 Setting the Stage for a Deeper Exploration of Both Conditions
- 2 Understanding Type 1 Diabetes: How It Begins, Why It Happens, and What It Means for the Body
- 3 Understanding Type 2 Diabetes: How It Develops, Why It Happens, and How the Body Tries to Cope
- 3.1 What Type 2 Diabetes Really Is: A Metabolic Condition Rooted in Insulin Resistance
- 3.2 How Insulin Resistance Slowly Develops Long Before Blood Sugar Rises
- 3.3 Why the Body Stores More Fat During Insulin Resistance and How This Affects Type 2 Diabetes
- 3.4 Why Type 2 Diabetes Often Feels Gradual and Confusing
- 3.5 How the Body Tries to Adapt When Insulin Resistance Deepens
- 4 Type 1 vs Type 2 Diabetes: Understanding the Key Differences With Emotional Clarity and Simple Medical Logic
- 4.1 How the Origins of Type 1 and Type 2 Diabetes Differ at the Deepest Biological Level
- 4.2 How Insulin Levels Differ Dramatically Between the Two Types
- 4.3 How Symptoms Tend to Appear: Sudden in Type 1, Gradual in Type 2
- 4.4 How Age of Onset Differs, and Why It Matters Less Than People Think
- 4.5 Why Treatment Strategies Differ So Strongly Between Type 1 and Type 2 Diabetes
- 5 Living With Type 1 vs Living With Type 2 Diabetes: How Daily Life, Emotional Experience, and Self-Care Differ
- 5.1 How Daily Management Differs Between Type 1 and Type 2 Diabetes
- 5.2 How Emotional Stress Feels Different in Type 1 and Type 2 Diabetes
- 5.3 How Diet Plays a Different Role in Type 1 and Type 2 Diabetes Management
- 5.4 How Physical Activity Influences Type 1 and Type 2 Diabetes Differently
- 5.5 How Medication Approaches Differ Between the Two Types
- 6 Summary of Type 1 vs Type 2 Diabetes — And a Final Reflection on Hope, Healing, and Understanding
- 6.1 Bringing the Differences Together With Calm and Clarity
- 6.2 Why Neither Type of Diabetes Defines a Person’s Worth or Strength
- 6.3 How Understanding the Differences Helps Reduce Fear and Increase Confidence
- 6.4 Why Hope Plays a Central Role in Managing Both Types of Diabetes
- 6.5 A Reflective and Inspiring Conclusion: Understanding as a Path to Empowerment
- 6.6 FAQs With Answers
Learn the clear difference between Type 1 and Type 2 diabetes in simple, compassionate language. Understand causes, symptoms, and treatment explained for beginners.
Read DISCLAIMER
The material presented here is for general informational and educational purposes only and is not medical advice. Although we attempt to provide current and accurate information, this blog should not be used as a replacement for professional medical consultation, diagnosis, or treatment. In all cases, consult your physician or an accredited medical practitioner with regards to any medical condition or treatment. Do not ignore professional medical advice or wait for it on the basis of information provided by this blog. In a medical emergency, call emergency services immediately.
Why Learning the Difference Matters More Than Most People Realize
There are moments in life when understanding something deeply can bring not just clarity but also comfort, especially when that understanding is connected to health, wellbeing, and the rhythms of the human body. Diabetes is one such topic, because even though it is widely spoken about, many people still feel uncertain, confused, or overwhelmed when trying to understand the difference between Type 1 and Type 2 diabetes. These two conditions share the same name, yet they are profoundly different in their origins, their progression, and the way the body responds to them. This confusion sometimes leads to fear or misunderstandings, and people may blame themselves unnecessarily or feel anxious about symptoms they do not fully comprehend. A gentle, clear explanation can help remove that fear, giving individuals a sense of grounding and reassurance that knowledge does not have to be frightening but can instead be empowering.
Understanding the difference between Type 1 and Type 2 diabetes is important because it allows people to appreciate how uniquely the body functions and how differently it can struggle. The human body is incredibly intelligent and always trying to protect and balance itself, yet the reasons it develops Type 1 diabetes are not the same reasons it develops Type 2 diabetes. These two conditions are not caused by the same issues, do not respond to the same treatments, and do not follow the same progression, yet they both revolve around the hormone insulin, which plays a central role in how the body uses glucose for energy. By learning about the differences in a slow, calming manner, individuals can replace worry with understanding and replace confusion with confidence.
When we explore these conditions with empathy, rather than clinical detachment, it becomes easier to absorb the information because the mind feels safe and open to learning. This emotional safety is essential because diabetes can feel intimidating, especially when terms like insulin deficiency, autoimmune destruction, insulin resistance, or chronic metabolic disorder come into the conversation. A warm and compassionate approach helps soften these technical ideas so they can be understood by anyone, even someone who has never studied biology before. This blog aims to offer such an explanation—one that embraces clarity while honoring the emotional experience of learning about a condition that affects so many individuals worldwide.
What Diabetes Really Means: Understanding the Foundation Before Exploring the Differences
Before exploring the specific differences between Type 1 and Type 2 diabetes, it is important to understand what diabetes itself truly means on the most basic biological level. Diabetes is a condition where the body struggles to regulate glucose, the simple sugar that acts as the primary fuel for every cell. Glucose is essential for survival because it provides energy for the brain, the muscles, the organs, and the entire system that keeps the body functioning. However, glucose cannot enter the cells without insulin, which acts as a guide or a key that helps glucose move out of the bloodstream and into the tissues where it is needed. When insulin is not available, or when the cells do not respond to insulin properly, glucose begins to accumulate in the blood instead of being used efficiently.
The word “diabetes” does not describe a single problem but rather a shared outcome: high blood sugar. What leads to this outcome differs greatly between Type 1 and Type 2 diabetes. In Type 1 diabetes, the body cannot produce insulin at all because the immune system mistakenly destroys the cells in the pancreas that make insulin. This leads to a state where the body is completely dependent on external insulin to survive. In Type 2 diabetes, the body usually produces insulin, sometimes even in large amounts, but the cells no longer respond to it correctly, creating a state known as insulin resistance. Over time, the pancreas becomes exhausted and produces less insulin, worsening the condition.
Understanding this foundational difference prepares the mind to grasp the deeper distinctions between Type 1 and Type 2 diabetes without feeling overwhelmed. It creates a sense of structure, allowing individuals to see that both conditions involve insulin but in very different ways. This clarity helps dissolve misconceptions and gives individuals the ability to speak confidently about diabetes, whether they are learning for themselves, supporting a loved one, or simply expanding their knowledge for personal wellbeing.
The Emotional Weight of the Diagnosis and Why Understanding Brings Relief
Whether someone hears the word “diabetes” for themselves or for someone they care about, the emotional impact can be significant, even if they do not say so out loud. The condition carries a sense of seriousness that touches people deeply, and many individuals fear what the future may look like or wonder whether they have done something wrong. This emotional response is completely normal, because diabetes involves long-term care and lifelong awareness, and such responsibilities can feel heavy at first. However, understanding the condition—truly understanding it in a gentle, human-centered way—can reduce this emotional load dramatically. Knowledge transforms fear into clarity, and clarity brings a sense of control.
When individuals understand the differences between Type 1 and Type 2 diabetes, they are suddenly able to make sense of what their bodies are experiencing rather than feeling lost in medical language. They begin to see that Type 1 diabetes is not caused by lifestyle or choices but by an autoimmune process beyond their control. Similarly, they understand that Type 2 diabetes is not an instant failure of the body but a slow metabolic shift influenced by many factors, including stress, sleep, genetics, inflammation, and hormonal changes. This understanding reduces self-blame, replaces guilt with compassion, and creates space for healthier emotional responses.
Learning about diabetes in a calm and supportive way also helps individuals reconnect with their bodies, realizing that the body is not their enemy but an intelligent system that requires support and care. It helps people appreciate that diabetes management is not a punishment but a pathway toward stability and safety. With this emotional foundation, individuals feel less overcome by the diagnosis and more empowered to take gentle steps that support their health. Understanding becomes the beginning of healing, even before any physical change occurs.
Why Comparing Type 1 and Type 2 Diabetes Can Be Confusing Without a Clear Framework
Many people feel confused when hearing about the two major types of diabetes because they hear the same words—blood sugar, insulin, glucose, pancreas—used in both discussions. Without a clear, compassionate explanation, it is easy to assume that Type 1 and Type 2 diabetes are simply different versions of the same condition, when in reality they are fundamentally different in origin, development, and treatment. This confusion creates anxiety, especially for beginners who are trying to understand the difference for the first time. The human mind needs structure when learning new information, especially when that information relates to health, and without structure, everything feels jumbled and overwhelming.
A clear framework helps individuals understand that Type 1 diabetes is an autoimmune condition where insulin production is nearly absent, while Type 2 diabetes is a metabolic condition where insulin is present but not used effectively. This structured understanding shows that although both conditions involve insulin and blood sugar regulation, they operate through very different mechanisms. With this clarity, people can approach the topic with confidence rather than uncertainty.
This framework also helps individuals understand why treatments differ so dramatically between the two types. Type 1 diabetes always requires insulin because the body cannot produce it, while Type 2 diabetes may initially be managed with lifestyle changes and medications that improve insulin sensitivity. Understanding these distinctions prevents misconceptions, reduces stigma, and helps individuals communicate accurately with healthcare professionals. It empowers beginners to approach diabetes education with openness instead of fear, creating a safe and supportive learning experience.
Setting the Stage for a Deeper Exploration of Both Conditions
Before diving into the deeper distinctions between Type 1 and Type 2 diabetes, it is important to prepare the mind for a journey that is both informative and emotionally grounding. The goal is not just to list medical differences but to create an understanding that feels gentle, compassionate, and respectful of the emotional experience that often accompanies learning about diabetes. This preparation helps individuals feel safe, allowing them to absorb information at a comfortable pace rather than feeling overwhelmed by technical details.
As we continue, we will explore Type 1 diabetes and Type 2 diabetes in depth—how they develop, how they differ, how they affect the body, and how each condition is managed. Every explanation will be delivered in simple, warm, patient-friendly language, ensuring that even beginners feel supported and understood. Each part of this blog will build upon the last, creating a layered understanding that grows naturally and calmly, without pressure or complexity.
This journey is not just about learning the differences between the two types of diabetes; it is about developing a sense of confidence, awareness, and emotional clarity about how the body works. By the end of this blog, individuals will feel equipped with knowledge that empowers rather than frightens, knowledge that can help them care for themselves or support others with compassion. And this begins now—with Part 1 complete and the deeper exploration ready to unfold.
Understanding Type 1 Diabetes: How It Begins, Why It Happens, and What It Means for the Body
What Type 1 Diabetes Really Is: A Gentle Explanation for Beginners
Type 1 diabetes is often misunderstood, and many people feel confused when trying to grasp how it actually develops, especially since it behaves so differently from Type 2 diabetes. To truly understand Type 1 diabetes, we must begin with the idea that the body has an immune system designed to protect us from anything that does not belong inside us, such as viruses or bacteria. This immune system is powerful, intelligent, and constantly alert, identifying and eliminating harmful intruders with remarkable precision. But in Type 1 diabetes, something unusual happens: the immune system mistakenly targets and destroys the insulin-producing beta cells in the pancreas, believing they are foreign even though they are a natural part of the body. This mistake is known as an autoimmune reaction, and it is not caused by anything a person did or did not do. It is not the result of diet, lifestyle, weight, or personal choices. It is simply an instance in which the immune system becomes confused and attacks the very cells responsible for producing insulin.
As these insulin-producing cells are gradually destroyed, the body loses its ability to create insulin, the hormone that helps glucose move from the bloodstream into the cells. Without insulin, glucose cannot enter the cells, and as a result, it begins to build up in the blood. This leads to high blood sugar levels, which can become dangerous if not managed. People with Type 1 diabetes must therefore rely on insulin injections or insulin pumps for survival, because the body no longer produces insulin on its own. Understanding this process helps replace fear and guilt with clarity and compassion, allowing individuals to appreciate that Type 1 diabetes is not anyone’s fault. It is not the result of poor decisions or lack of care; it is a condition that arises from the body’s immune system acting in a way that it was not intended to. Knowing this helps reduce stigma and encourages a more empathetic understanding of the condition.
Why the Immune System Attacks the Pancreas in Type 1 Diabetes
The question many beginners ask is why the immune system becomes confused in the first place. Unfortunately, science does not yet have a single answer, but research suggests that a combination of factors—genetic, environmental, and possibly viral—may influence the immune system’s behavior. Some individuals may carry certain genes that make them more likely to experience autoimmune conditions, and in these individuals, certain triggers may activate the immune response that leads to Type 1 diabetes. These triggers may include viral infections, stressors, environmental exposures, or immune system miscommunication that happens beyond conscious control. Importantly, none of these triggers are caused by personal choices or lifestyle habits. A person cannot “cause” Type 1 diabetes by eating sugar, gaining weight, or living a certain way. This understanding brings emotional relief because it removes the sense of blame that people often carry when trying to make sense of the diagnosis.
As the autoimmune process continues, the immune system slowly destroys more and more beta cells. In the early stages, the pancreas may still be able to produce small amounts of insulin, which is why some individuals experience what is called the “honeymoon phase,” a brief period where insulin needs seem lower than expected. However, this phase is temporary, because the underlying autoimmune attack continues, eventually eliminating nearly all insulin-producing cells. Once insulin production becomes insufficient, the body enters a state where insulin must be replaced externally. Understanding this process helps individuals realize that Type 1 diabetes is fundamentally a condition of insulin absence, not insulin resistance. This distinction is essential for beginners because it provides the foundation for understanding why treating Type 1 diabetes requires insulin therapy, not oral medications or lifestyle management alone.
How the Body Changes When Insulin Is No Longer Produced
When the pancreas stops producing insulin, the effects ripple throughout the body in profound ways. Glucose begins to accumulate in the bloodstream because it cannot enter the cells without insulin’s guidance. The cells, meanwhile, become starved of energy despite the abundance of glucose circulating outside them, creating a state of internal confusion where the body feels both overloaded and deprived at the same time. This is why people with untreated Type 1 diabetes may feel extremely tired, thirsty, and hungry, even though they are eating and drinking normally. The body tries to compensate by breaking down fat and muscle for energy, which can lead to rapid weight loss despite no intentional changes in diet or activity. These changes are not a matter of discipline or control; they are the body’s attempt to survive without insulin.
Over time, the high levels of glucose in the blood begin to pull water out of the tissues, contributing to dehydration and increased urination. This cycle becomes overwhelming for the body, and without treatment, it can lead to a dangerous condition called diabetic ketoacidosis, which requires immediate medical care. Understanding these changes helps individuals see that insulin is far more than a hormone involved in blood sugar control; it is essential for energy, hydration, cellular function, and overall survival. This knowledge encourages compassion and reminds individuals that managing Type 1 diabetes is not optional but vital for sustaining life. It also helps people recognize the importance of consistent insulin therapy and the role it plays in restoring balance to the body.
Living With Type 1 Diabetes: A Partnership Between Knowledge and Care
Although Type 1 diabetes requires lifelong insulin therapy, it is not a condition defined only by challenges. With awareness, education, and supportive care, individuals can learn to manage their blood sugar, understand their body’s signals, and maintain stability in ways that allow for full, meaningful lives. The key to living with Type 1 diabetes lies in developing a partnership with the body—a partnership built on patience, understanding, and a willingness to learn. This involves learning how food, stress, activity, illness, and emotions influence blood sugar and adjusting insulin doses accordingly. Such learning does not happen overnight, and beginners often feel overwhelmed at first, but with time, experience brings confidence, clarity, and strength.
This partnership also requires emotional care, because managing a condition that needs daily attention can be exhausting. Understanding the emotional struggles associated with Type 1 diabetes is essential, as feelings of frustration, fear, or overwhelm are natural responses to a demanding condition. Recognizing these emotions allows individuals to seek support, speak openly about their experiences, and approach self-care with kindness. Type 1 diabetes becomes less frightening when individuals understand its nature and build a compassionate relationship with themselves. Knowledge becomes a tool of empowerment rather than pressure, and self-care becomes a gentle practice rather than a burden.
Understanding Type 2 Diabetes: How It Develops, Why It Happens, and How the Body Tries to Cope
What Type 2 Diabetes Really Is: A Metabolic Condition Rooted in Insulin Resistance
Type 2 diabetes is a condition that often develops gradually, making it quite different from Type 1 diabetes, which has a more sudden and autoimmune-based origin. In Type 2 diabetes, the body still produces insulin—often in large amounts—but the cells no longer respond to it the way they should, creating a state known as insulin resistance. When the cells become resistant, insulin cannot open the “doors” of the cells as effectively, leaving glucose circulating in the bloodstream instead of being used for energy. In response, the pancreas works harder and harder, producing more insulin in an attempt to force glucose into the cells. For a while, this extra effort works, keeping blood sugar levels normal or only slightly elevated. But with time, the pancreas becomes strained and exhausted, and its ability to produce insulin decreases. This is when blood sugar begins rising consistently, marking the transition into prediabetes and eventually Type 2 diabetes.
Understanding this process helps beginners see that Type 2 diabetes is not caused by a lack of insulin but by the body’s inability to use insulin well. This distinction is important because it informs the way the condition is treated and the way individuals understand their symptoms. Many people wrongly assume that Type 2 diabetes happens suddenly or that it appears only in certain kinds of individuals, but the truth is that it can affect anyone because it is influenced by a combination of genetics, stress, sleep quality, hormonal changes, diet, activity levels, and overall metabolic health. This realization helps reduce guilt, as beginners understand that Type 2 diabetes does not reflect weakness, irresponsibility, or moral failure but rather a complex internal imbalance that develops silently over time. Understanding the biological basis makes the condition less frightening and more approachable, creating space for learning and healing.
How Insulin Resistance Slowly Develops Long Before Blood Sugar Rises
One of the most important things to understand about Type 2 diabetes is that insulin resistance begins many years before a diagnosis is ever made. During this long hidden phase, the pancreas compensates by producing more and more insulin to overcome the resistance, keeping blood sugar within a normal range. Because blood sugar remains normal for so long, people often believe their health is stable, even though their metabolic system is quietly struggling. The early signs of insulin resistance—such as fatigue, cravings, weight changes, sleep disturbances, and mood fluctuations—are easily misattributed to stress or aging. Most people never realize that these early signals are warnings that the cells are no longer responding to insulin effectively. As insulin resistance deepens, the pancreas becomes increasingly burdened, and insulin levels remain chronically high, which can lead to increased fat storage, especially around the abdomen.
Over time, the pancreas slowly begins to lose its ability to keep up with the growing demand, and blood sugar levels start to rise. This shift does not happen abruptly; it is the result of years of metabolic strain, inflammation, and hormonal imbalance. It is only at this stage that blood tests reveal prediabetes or Type 2 diabetes, even though the condition has been developing silently for a long time. Understanding this progression is essential because it helps individuals recognize that early intervention—long before symptoms become severe—can reverse insulin resistance and restore balance. This knowledge empowers people to make gentle changes that support the pancreas, reduce inflammation, improve insulin sensitivity, and prevent further decline.
Why the Body Stores More Fat During Insulin Resistance and How This Affects Type 2 Diabetes
One of the most challenging emotional aspects of Type 2 diabetes is the way insulin resistance influences weight gain, especially in the abdominal area. When insulin levels remain chronically high, the body receives a signal to store energy rather than burn it, particularly in the form of fat. This is not a matter of willpower, discipline, or personal failure; it is a direct hormonal response to insulin resistance. Fat cells themselves begin releasing inflammatory signals that worsen resistance, creating a cycle where the body becomes more resistant to insulin as fat storage increases. Many beginners feel frustrated when they notice that their weight is increasing despite eating modestly or trying to stay active, not realizing that hormonal patterns—not behavior—are shaping their weight journey.
Additionally, the liver plays a significant role in this process. When the body becomes insulin-resistant, the liver converts more glucose into fat, contributing to fatty liver disease, which further weakens insulin sensitivity. This interconnected series of events creates a metabolic environment where the body has difficulty using energy efficiently, leading to fatigue, cravings, heaviness, and emotional distress. Understanding these biological changes helps individuals replace frustration with self-compassion, recognizing that weight changes are not a personal failure but a predictable outcome of hormonal imbalance. This clarity encourages individuals to pursue healing from a place of kindness, patience, and understanding rather than pressure or guilt.
Why Type 2 Diabetes Often Feels Gradual and Confusing
Unlike Type 1 diabetes, which often presents suddenly with intense symptoms, Type 2 diabetes develops gradually, and the early signs may feel subtle or easily overlooked. People may notice changes in energy, hunger patterns, mood stability, digestion, or sleep, but these changes rarely seem severe enough to trigger concern. Instead, individuals often assume they are simply tired, stressed, aging, or going through temporary fluctuations. This gradual progression makes Type 2 diabetes difficult to detect without routine screening, which is why many people discover it only when blood work reveals elevated glucose levels. This can create a sense of shock or disbelief, because the individual may have felt relatively normal even as metabolic changes were unfolding quietly behind the scenes.
Understanding why Type 2 diabetes feels gradual helps individuals process the diagnosis with less confusion and more emotional stability. It helps them see that their body was working hard for many years to maintain balance under increasing strain and that the diagnosis simply reflects the moment when their system could no longer compensate. This understanding removes the guilt that often accompanies the diagnosis and gives beginners the clarity they need to focus on healing rather than self-blame. When people understand that Type 2 diabetes is a process, not a sudden event, they feel more empowered to slow down, breathe, and make thoughtful changes that support long-term health.
How the Body Tries to Adapt When Insulin Resistance Deepens
One of the most remarkable things about the human body is its ability to adapt, even when facing internal challenges like insulin resistance. In Type 2 diabetes, these adaptations are a reflection of the body’s attempt to protect itself and maintain balance, even when conditions are far from ideal. For example, the pancreas increases insulin production to compensate for reduced cellular sensitivity, trying to keep blood sugar stable for as long as possible. Muscles may adjust their glucose absorption, the liver may alter glucose production, and hormonal pathways may shift in an attempt to create stability. Despite these efforts, however, the body eventually reaches a point where it cannot compensate any further, especially when inflammation, stress, poor sleep, or genetic tendencies add to the metabolic burden.
Seeing Type 2 diabetes through the lens of adaptation rather than failure helps individuals appreciate the incredible work their bodies have done to protect them throughout the process. It reminds them that their bodies have not betrayed them; instead, their bodies have done everything possible to maintain equilibrium in the face of metabolic stress. This perspective not only creates emotional relief but also encourages individuals to support their bodies with habits that strengthen insulin sensitivity, reduce inflammation, and restore metabolic balance. When people understand how hard their bodies have been working, they are often more motivated to care for themselves with patience and gentleness.

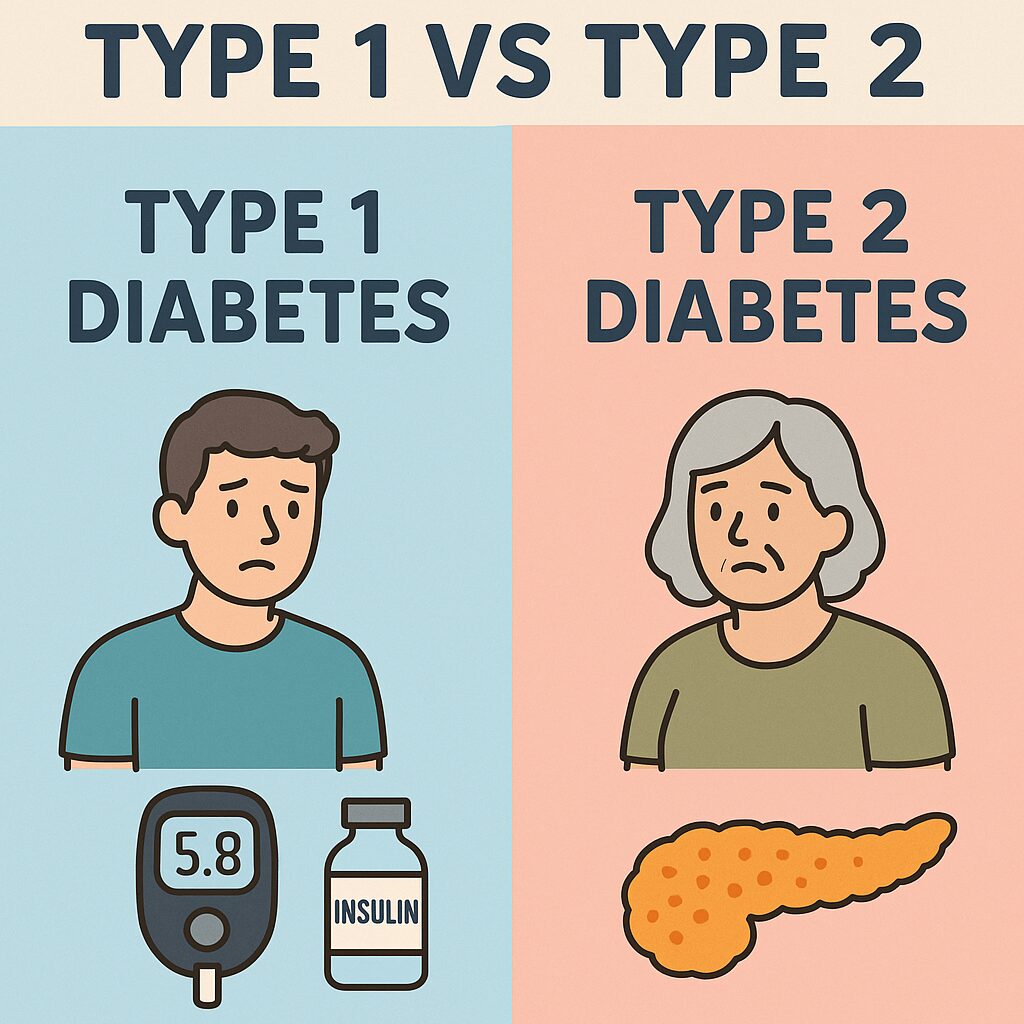
Type 1 vs Type 2 Diabetes: Understanding the Key Differences With Emotional Clarity and Simple Medical Logic
How the Origins of Type 1 and Type 2 Diabetes Differ at the Deepest Biological Level
The most important difference between Type 1 and Type 2 diabetes lies in the very origin of each condition, and understanding this difference provides a profound sense of clarity for beginners. Type 1 diabetes begins when the immune system mistakenly destroys the insulin-producing beta cells in the pancreas, leaving the body unable to produce insulin. This destruction is not caused by lifestyle, diet, weight, or personal decisions; it is an autoimmune process that can occur even in individuals who otherwise appear perfectly healthy. In contrast, Type 2 diabetes develops because the cells of the body become resistant to insulin, meaning insulin is present but no longer effective. Over time, the pancreas becomes overwhelmed trying to produce enough insulin to overcome this resistance, eventually wearing down and producing less.
This distinction shapes everything that follows—from symptoms to treatment to long-term management. In Type 1 diabetes, the pancreas produces almost no insulin, making insulin therapy absolutely essential for survival. In Type 2 diabetes, insulin is present, sometimes even in large amounts, but the body cannot use it effectively. This difference helps explain why Type 2 diabetes can sometimes be improved or reversed with lifestyle adjustments, while Type 1 diabetes requires lifelong insulin therapy regardless of diet, exercise, or habits. Understanding these root differences removes confusion and reduces the emotional weight many individuals feel when trying to make sense of how diabetes develops. It also helps people recognize that every body has its own unique challenges, and comparing the two conditions without this clarity only leads to misunderstanding.
How Insulin Levels Differ Dramatically Between the Two Types
Another major difference between Type 1 and Type 2 diabetes lies in the way insulin behaves within the body. In Type 1 diabetes, the immune system has destroyed most or all of the beta cells responsible for creating insulin, leaving the body with little to no insulin production. This means glucose cannot enter the cells at all unless insulin is provided externally. The body becomes dependent on insulin injections or pumps as its only means of regulating blood sugar, and this dependence is lifelong.
In Type 2 diabetes, insulin is still being produced—often in higher levels than normal—because the pancreas is trying to push glucose into cells that are increasingly resistant. Early in the condition, insulin levels are actually higher than those of a healthy person, yet the body still struggles to regulate blood sugar because the cells are not responding efficiently. Eventually, the pancreas becomes fatigued from years of overproduction and begins producing less insulin, leading to rising blood sugar levels. Understanding this contrast helps individuals grasp why the treatments differ so much: Type 1 diabetes requires external insulin from the start, while Type 2 diabetes may begin with lifestyle adjustments and medications that improve insulin sensitivity. This distinction makes it easier for beginners to understand why insulin use in Type 2 diabetes varies widely from person to person and why insulin becomes necessary only when the pancreas can no longer keep up.
How Symptoms Tend to Appear: Sudden in Type 1, Gradual in Type 2
Type 1 and Type 2 diabetes also differ greatly in how their symptoms begin, and this difference reflects the underlying biological processes. Type 1 diabetes usually appears suddenly, often over a short period of days or weeks, because the insulin-producing cells are rapidly destroyed by the immune system. Once the body can no longer produce insulin, blood sugar rises quickly, leading to intense symptoms such as extreme thirst, frequent urination, rapid weight loss, fatigue, and dehydration. The sudden onset of Type 1 diabetes can feel alarming and overwhelming, as the body transitions abruptly from balanced glucose control to complete insulin dependence.
Type 2 diabetes, in contrast, develops slowly and quietly, sometimes over many years, as insulin resistance increases and the pancreas struggles to keep up with demand. The early symptoms may be subtle—like mild fatigue, slight hunger changes, or gradual weight gain—and often remain unnoticed because they can be easily attributed to stress or aging. As the condition progresses, symptoms become more noticeable, including increased thirst, frequent urination, blurred vision, and decreased energy. Because these changes build slowly, many people do not realize they have Type 2 diabetes until blood tests reveal elevated glucose levels. Understanding these differences in symptom progression helps beginners recognize why Type 1 diabetes feels abrupt and urgent, while Type 2 diabetes feels gradual and confusing. It also helps remove the emotional pressure that often accompanies late detection of Type 2 diabetes.
How Age of Onset Differs, and Why It Matters Less Than People Think
Another key difference between Type 1 and Type 2 diabetes is the age at which they typically appear. Type 1 diabetes has historically been known as “juvenile diabetes” because it often appears in childhood or adolescence. However, it can occur at any age, including adulthood, even though childhood onset remains more common. Type 2 diabetes, on the other hand, has traditionally been associated with adults, particularly those over 40, because insulin resistance tends to deepen with age. However, in recent decades, Type 2 diabetes has become increasingly common in younger individuals due to changes in lifestyle patterns, stress levels, sleep quality, and overall metabolic health.
These age patterns are common but not absolute, and beginners should understand that diabetes type cannot be determined solely by age. Many young adults receive a Type 2 diabetes diagnosis, while some adults receive a Type 1 diagnosis later in life. This overlap often causes confusion, which is why proper testing is essential to distinguish between the two conditions. Understanding that age is not the defining factor helps individuals feel less confused or misled when their diagnosis does not fit traditional assumptions. It helps them see that diabetes develops based on biology, not stereotypes, and that the body’s internal processes are far more nuanced than age categories suggest.
Why Treatment Strategies Differ So Strongly Between Type 1 and Type 2 Diabetes
Because the origins of the two types differ so profoundly, the treatment strategies also differ in ways that beginners must understand clearly to avoid confusion. In Type 1 diabetes, the body cannot produce insulin at all, making external insulin absolutely necessary for survival. Without insulin, the cells cannot receive glucose, and the body cannot function. This means individuals with Type 1 diabetes rely on insulin injections or pumps for every meal, every day, throughout life. Insulin therapy is not optional in Type 1 diabetes; it is the core of treatment.
In Type 2 diabetes, however, treatment begins with improving insulin sensitivity through lifestyle adjustments, medications, or weight reduction. These interventions help the body use insulin more effectively, reducing the burden on the pancreas. Some individuals may eventually require insulin therapy if their pancreas becomes too fatigued to produce enough insulin. The timing of insulin therapy in Type 2 diabetes varies widely from person to person, depending on genetics, lifestyle, inflammation levels, and the progression of insulin resistance. Understanding these differences helps beginners see why two people with “diabetes” may have completely different treatment plans. It also helps alleviate anxiety about insulin, as individuals realize that insulin therapy reflects the underlying biology of the condition rather than a personal failure.
Living With Type 1 vs Living With Type 2 Diabetes: How Daily Life, Emotional Experience, and Self-Care Differ
How Daily Management Differs Between Type 1 and Type 2 Diabetes
Daily life with diabetes is shaped by the type of diabetes a person has, and understanding these differences helps beginners appreciate both the unique challenges and the unique strengths required for each condition. In Type 1 diabetes, daily management revolves around insulin because the body cannot produce it at all. This means individuals must carefully monitor blood sugar throughout the day, adjust insulin doses based on food intake, activity, stress, and emotions, and consistently remain aware of how their body responds to even small changes. Without insulin, the body cannot use glucose, so every meal becomes a calculation, every activity becomes a variable, and every day requires attentiveness. This constant awareness can feel overwhelming at first, but over time many individuals develop a rhythm that helps them navigate their needs with increasing confidence and calm.
In Type 2 diabetes, daily management varies widely because the body still produces insulin and may respond to treatment in different ways. Some individuals manage their condition through improved activity levels, nourishing meals, better sleep, and reduced stress—changes that help insulin become more effective again. Others may use oral medications that either increase insulin sensitivity, reduce glucose production in the liver, or help the pancreas release insulin more efficiently. In some cases, insulin therapy becomes necessary as the condition progresses. Because Type 2 diabetes is influenced by insulin resistance rather than insulin deficiency, daily life often centers on supporting the body’s ability to use insulin well. This means lifestyle plays a large role, but lifestyle is not the cause of the condition; it is simply a tool for improving the body’s response. Understanding this helps individuals approach each day with compassion rather than blame, recognizing that diabetes management is an ongoing relationship with the body rather than a constant struggle against it.
How Emotional Stress Feels Different in Type 1 and Type 2 Diabetes
Emotional stress affects all forms of diabetes, but the way stress shows up and the way it is felt can differ significantly between Type 1 and Type 2 diabetes due to the underlying biological differences. In Type 1 diabetes, stress often affects blood sugar rapidly and noticeably because insulin levels are entirely dependent on external administration. Emotional tension, fear, excitement, and even minor disruptions can cause blood sugar fluctuations that require immediate attention. This creates a sense of heightened awareness, where individuals may feel pressure to remain vigilant in order to prevent sudden highs or lows. The emotional weight of this responsibility can be heavy, especially for those newly diagnosed, because it is not only physical stability that needs managing but the emotional sensitivity that comes with unpredictable glucose changes. Over time, many individuals develop a deep emotional resilience, learning to trust their ability to respond and adapt, but the emotional experience remains uniquely intense because the stakes are immediate.
In Type 2 diabetes, emotional stress influences blood sugar more gradually but no less importantly. Stress hormones such as cortisol and adrenaline increase insulin resistance, making the body less responsive to insulin and causing blood sugar to rise. These changes may not feel as sudden as they do in Type 1 diabetes, but they accumulate over time, creating patterns of fatigue, cravings, irritability, or mental fog that reflect the metabolic strain. The emotional experience of Type 2 diabetes often includes frustration, confusion, or guilt, as individuals may wonder why their blood sugar fluctuates despite seemingly consistent habits. Understanding that stress directly affects insulin resistance helps individuals release self-blame and approach their emotional world with greater gentleness. It also highlights the importance of emotional self-care as a meaningful part of diabetes management, regardless of type.
How Diet Plays a Different Role in Type 1 and Type 2 Diabetes Management
Food is important in both types of diabetes, but its role differs dramatically depending on whether the issue is insulin absence or insulin resistance. In Type 1 diabetes, diet does not determine whether insulin is produced, because the pancreas cannot make insulin at all. Instead, diet matters because carbohydrates influence how much insulin needs to be taken externally. This means individuals with Type 1 diabetes often focus more on balancing their meals with appropriate insulin doses rather than avoiding specific foods altogether. The goal is not to restrict but to understand how carbohydrates affect blood sugar and how insulin can be used to bring the body back into balance. This creates a relationship with food that is more mathematical than metabolic, where each meal becomes an opportunity to adjust insulin and maintain stability.
In Type 2 diabetes, diet plays a more direct metabolic role because the body still produces insulin but struggles to use it effectively. Certain foods can increase insulin resistance, while others improve it, making nutritional choices a powerful tool for healing. Balanced meals help stabilize blood sugar, reduce inflammation, support liver health, and lighten the workload on the pancreas. Many individuals notice significant improvements in their symptoms when their eating patterns align with stabilizing insulin sensitivity rather than triggering insulin spikes. However, this does not mean that Type 2 diabetes is caused by diet alone; it simply reflects that food interacts deeply with insulin resistance, giving individuals a way to support their body through nourishment. Understanding these distinctions helps beginners see that dietary guidance must be tailored to the type of diabetes, not generalized across both conditions.
How Physical Activity Influences Type 1 and Type 2 Diabetes Differently
Movement is essential for everyone, but in the context of diabetes, its impact depends on whether the body lacks insulin or resists it. In Type 1 diabetes, physical activity lowers blood sugar rapidly because muscles can absorb glucose independently of insulin when they contract. This means individuals must monitor their glucose closely during and after exercise to avoid sudden drops. Activities that require prolonged effort may cause delayed lows, while high-intensity exercise may briefly raise blood sugar due to stress hormones. This creates a complex relationship with movement, one that requires awareness, planning, and emotional steadiness. Yet for many individuals with Type 1 diabetes, movement also becomes a source of empowerment, helping them feel strong, grounded, and connected to their bodies.
In Type 2 diabetes, physical activity is one of the most powerful tools for improving insulin sensitivity. When muscles contract regularly, they begin absorbing glucose more efficiently, reducing the need for high insulin levels. Over time, consistent movement helps reverse insulin resistance, lower inflammation, support weight management, and improve overall metabolic health. The changes are gradual but profound, making movement not just a supportive habit but a metabolic medicine. Individuals often feel encouraged when they start noticing improvements in energy, mood, and glucose stability, which reinforces their motivation. Understanding these differences helps beginners appreciate why exercise guidelines are not one-size-fits-all and must reflect the biology of the diabetes type.
How Medication Approaches Differ Between the Two Types
Medication plays a significant role in diabetes care, but the approach varies widely depending on whether the body lacks insulin entirely or struggles to use insulin effectively. In Type 1 diabetes, insulin is not merely a treatment; it is a life-sustaining requirement. No oral medication or lifestyle change can replace the need for insulin because the pancreas no longer produces it. Insulin therapy may be delivered through injections or insulin pumps, and the type and timing of insulin must be tailored to each individual’s daily patterns. People with Type 1 diabetes often learn to adjust doses based on meals, physical activity, hormones, emotions, and overall wellbeing. This requires attentiveness but also empowers individuals to understand their bodies in ways that are both profound and deeply personal.
In Type 2 diabetes, medication approaches vary enormously because the goals differ based on the stage of insulin resistance. Some medications help the liver release less glucose, some help muscles absorb glucose more effectively, and others make the pancreas release more insulin. Insulin may eventually become necessary if the pancreas becomes too fatigued to meet the body’s needs, but not everyone with Type 2 diabetes requires insulin. Understanding this variety helps beginners see that Type 2 diabetes is not a uniform condition but a spectrum, and treatment must be adjusted over time as the body’s responses change. This clarity helps individuals approach medication with confidence rather than fear, knowing that adjustments reflect the natural progression of the condition, not personal inadequacy.

Summary of Type 1 vs Type 2 Diabetes — And a Final Reflection on Hope, Healing, and Understanding
Bringing the Differences Together With Calm and Clarity
After exploring both Type 1 and Type 2 diabetes in depth, it becomes clear that these two conditions, though sharing the same name, come from entirely different biological pathways and require different approaches to care. Type 1 diabetes is rooted in an autoimmune reaction where the body no longer produces insulin at all, making external insulin essential for survival. Type 2 diabetes, on the other hand, begins with insulin resistance, meaning insulin is present but not used properly, leading to gradual strain on the pancreas and slowly rising blood sugar levels. While Type 1 diabetes often presents suddenly, Type 2 diabetes develops silently and gradually, sometimes over many years. These differences shape daily life, emotional experience, treatment needs, lifestyle support, and the rhythm of self-care for each individual.
Yet, despite these differences, both conditions share a common emotional landscape: the need for understanding, patience, compassion, and steady awareness. Both require individuals to listen to their bodies more closely than before, to observe how stress, sleep, food, and activity influence their daily wellbeing. Both require courage and a degree of emotional resilience, because managing a condition that affects the body every day can be overwhelming, especially at first. Understanding these differences not only helps individuals manage their own condition more confidently but also helps create a more empathetic world, where misconceptions and judgment are replaced with informed compassion. When the differences are clear, the fear surrounding diabetes softens, and the path forward feels more grounded and manageable.
Why Neither Type of Diabetes Defines a Person’s Worth or Strength
One of the most important truths about both Type 1 and Type 2 diabetes is that neither condition says anything about a person’s value, their intelligence, their discipline, or their emotional strength. Type 1 diabetes is not caused by anything a person did, and Type 2 diabetes is not a reflection of laziness, weakness, or lack of care. Both conditions develop because of biological factors that are far more complex than most people realize. Blame has no place here, and guilt only adds emotional weight that harms more than it helps. When individuals let go of the idea that diabetes reflects personal failure, they create space to approach their health from a place of compassion rather than pressure.
This shift in perspective is vital because diabetes management—whether Type 1 or Type 2—requires emotional steadiness and self-kindness. People do not heal by punishing themselves; they heal by understanding themselves. They heal by acknowledging what their bodies need and responding gently. They heal by accepting that learning how to manage diabetes takes time, patience, and ongoing effort, not perfection. When individuals embrace the truth that diabetes management is a journey rather than a test, they begin to cultivate resilience, trust, and confidence in their own abilities. This emotional freedom becomes as important as any treatment plan, because it allows individuals to move forward with hope rather than fear.
How Understanding the Differences Helps Reduce Fear and Increase Confidence
Many people experience fear when they first hear the word “diabetes,” but much of this fear comes from misinformation, assumptions, or a lack of understanding about what the condition truly involves. When the differences between Type 1 and Type 2 diabetes become clear, the fear begins to dissolve because understanding replaces uncertainty. Beginners who once felt overwhelmed by medical terms suddenly begin to see the logic behind the body’s responses. They learn why Type 1 diabetes requires insulin, why Type 2 diabetes involves insulin resistance, why symptoms differ, and why treatment plans must be personalized. This clarity brings calmness, and that calmness creates emotional space for learning, adapting, and improving.
Understanding the differences also empowers individuals to advocate for themselves in healthcare environments, ask the right questions, and participate in their treatment decisions with confidence. It helps loved ones offer meaningful support rather than assumptions. It helps society reduce stigma and judgment by recognizing that diabetes—regardless of type—is a complex condition shaped by biology, not blame. When confusion is replaced by understanding, the relationship between a person and their health becomes less frightening and more collaborative.
Why Hope Plays a Central Role in Managing Both Types of Diabetes
Despite their differences, both Type 1 and Type 2 diabetes share one crucial truth: the presence of hope. Type 1 diabetes has transformed dramatically over the years, with modern insulin therapies, continuous glucose monitors, and pumps offering greater ease, flexibility, and safety than ever before. Type 2 diabetes, similarly, can often be improved or even reversed in its early stages by supporting insulin sensitivity through nourishing habits, stress reduction, gentle movement, and improved sleep. Even when reversal is not possible, better management is always achievable.
Hope is not denial of challenges—it is the belief that challenges can be met with strength, learning, and steady care. It is the knowledge that the body responds beautifully to support, that the mind becomes stronger through understanding, and that emotional resilience grows with time. Hope gives individuals the courage to create new routines, to trust in medical guidance, and to stay committed even on difficult days. With hope, diabetes becomes not a limitation but a relationship—a relationship that requires patience, but one that can also bring greater awareness, deeper self-connection, and a profound appreciation of the body’s intelligence.
A Reflective and Inspiring Conclusion: Understanding as a Path to Empowerment
Understanding the difference between Type 1 and Type 2 diabetes is more than a lesson in biology; it is an invitation to see the human body with compassion, curiosity, and respect. When these two conditions are understood clearly, fear loses its grip, self-blame fades, and individuals can begin to approach their health with a gentle sense of empowerment. Knowledge becomes a form of emotional medicine, helping individuals feel stable, calm, and capable as they navigate daily life with diabetes. Whether someone is living with Type 1, living with Type 2, supporting a loved one, or simply learning to understand the body better, this clarity offers a powerful foundation for informed decisions and emotional peace.
Both Type 1 and Type 2 diabetes remind us of how intricate, adaptable, and resilient the body truly is. They remind us that healing is not a single act but a continuous relationship with our own wellbeing. They remind us that the body speaks to us—not through judgment but through signals, rhythms, and changes that reflect deeper needs. When individuals learn to listen gently, to respond with kindness, and to trust in their capacity to adapt, they discover that managing diabetes is not just a medical journey but a profound personal one.
In the end, the most important truth is this: diabetes does not take away a person’s ability to live fully, joyfully, or meaningfully. With understanding, compassion, guidance, and hope, every individual can create a life that honors both their body and their emotional resilience. Understanding the difference between Type 1 and Type 2 diabetes is the first step on that journey—a step toward clarity, strength, and the deep trust that healing is always possible.
FAQs With Answers
- What is the main difference between Type 1 and Type 2 diabetes?
The main difference lies in how the body handles insulin. In Type 1 diabetes, the immune system destroys insulin-producing cells, resulting in little or no insulin production. In Type 2 diabetes, the body still produces insulin, sometimes even in excess, but the cells become resistant to it. This means Type 1 is an insulin-deficiency condition, while Type 2 is an insulin-resistance condition.
- Does lifestyle cause Type 1 diabetes?
No, Type 1 diabetes is not caused by lifestyle, diet, or personal habits. It is an autoimmune condition where the immune system mistakenly attacks the pancreas. This process is not preventable and cannot be reversed. Understanding this removes blame and helps individuals focus on safe and supportive management.
- Why does Type 2 diabetes develop gradually?
Type 2 diabetes develops slowly because insulin resistance builds over years, often without noticeable symptoms. The pancreas compensates by producing more insulin until it becomes exhausted. This gradual shift means many people do not recognize the condition until blood tests reveal elevated glucose levels.
- Can Type 1 diabetes be reversed?
No, Type 1 diabetes cannot be reversed because the body permanently loses the ability to produce insulin. Insulin therapy is essential for survival. However, excellent management is possible with modern treatments like insulin pumps and continuous glucose monitors.
- Can Type 2 diabetes be reversed?
In many cases, early Type 2 diabetes and prediabetes can be improved or reversed through improved insulin sensitivity. Gentle lifestyle changes such as nourishing meals, consistent movement, deeper sleep, and stress reduction help the body use insulin more effectively. Reversal depends on how long the condition has existed and how fatigued the pancreas has become.
- Why do symptoms appear suddenly in Type 1 diabetes?
Type 1 diabetes symptoms appear abruptly because the immune system destroys insulin-producing cells rapidly. Without insulin, glucose cannot enter the cells, causing blood sugar levels to rise quickly. This leads to extreme thirst, weight loss, fatigue, and frequent urination within days or weeks.
- Why do symptoms appear slowly in Type 2 diabetes?
Type 2 diabetes progresses slowly because the body initially compensates for insulin resistance by producing extra insulin. Blood sugar remains normal for years before rising. This delay often leads people to overlook early signs like fatigue, cravings, or mild thirst.
- Do people with Type 1 diabetes always need insulin?
Yes, because the body no longer produces insulin at all. Insulin therapy is the foundation of survival for Type 1 diabetes. Without insulin, glucose cannot enter the cells, and the body cannot function.
- Do all people with Type 2 diabetes eventually need insulin?
Not always. Some individuals may manage Type 2 diabetes with lifestyle adjustments and medications that improve insulin sensitivity. Others may eventually require insulin if the pancreas becomes too fatigued. Treatment depends on progression, genetics, and overall metabolic health.
- Why does weight change differently in Type 1 versus Type 2 diabetes?
In Type 1 diabetes, rapid weight loss occurs because the body cannot use glucose for energy, so it breaks down fat and muscle. In Type 2 diabetes, insulin resistance leads to higher insulin levels, which encourage fat storage, especially around the abdomen. This makes weight loss more challenging.
- Why does stress affect both types of diabetes?
Stress increases cortisol, a hormone that raises blood sugar. In Type 1 diabetes, this can cause sudden spikes requiring insulin adjustments. In Type 2 diabetes, stress worsens insulin resistance, making blood sugar harder to control. Managing stress is therefore essential in both conditions.
- How does food affect Type 1 vs Type 2 diabetes?
In Type 1 diabetes, food influences how much insulin must be taken, but diet does not affect insulin production. In Type 2 diabetes, food has a deep metabolic effect because certain foods improve or worsen insulin resistance. Both types benefit from balanced meals but for different biological reasons.
- Why is physical activity important for both types?
Movement allows muscles to absorb glucose more effectively. In Type 1 diabetes, exercise lowers blood sugar quickly, requiring careful monitoring. In Type 2 diabetes, activity improves insulin sensitivity, making it one of the most powerful long-term therapies.
- Can Type 1 and Type 2 diabetes occur at any age?
Yes. Although Type 1 diabetes is more common in childhood and Type 2 diabetes more common in adulthood, both can occur at any age. Diagnosis must be based on testing, not assumptions about age.
- Does having diabetes mean life will be limited?
No. With proper understanding, modern treatments, emotional support, and consistent care, people with both Type 1 and Type 2 diabetes can live full, meaningful, healthy lives. The condition requires awareness, not fear, and management becomes easier with knowledge and compassionate guidance.